Programs
Information Box Group

Care of People Deprived of Housing Learn More
Our research in this area aims to understand the social determination of health and the brilliance of people and communities surviving and thriving in the face of structural violence.
Led by Robin Lennox and Claire Bodkin

Care of People Who Use Drugs Learn More
Our research studies novel hospital and community-based health interventions aimed at improving the health outcomes and healthcare experiences of people who use drugs.
Led by Robin Lennox
Full Scope Generalist MEDEd Research Lab Learn More
The Full Scope Generalist Medical Education (FSG Med Ed) Research Lab is grounded in the foundational idea that education matters. From this perspective, the FSG Med Ed Lab pursues studies that aim to emphasize, elucidate, and improve the relationship between health professional training and the healthcare delivered to patients and communities.
Led by Lawrence Grierson

Health TAPESTRY Learn More
Health TAPESTRY is a community-based program, led by primary care teams, that creates connections between trained health care volunteers, interprofessional health care teams, novel technology and community engagement through improved system navigation.
Led by David Price, Dee Mangin, Doug Oliver and Jessica Gaber
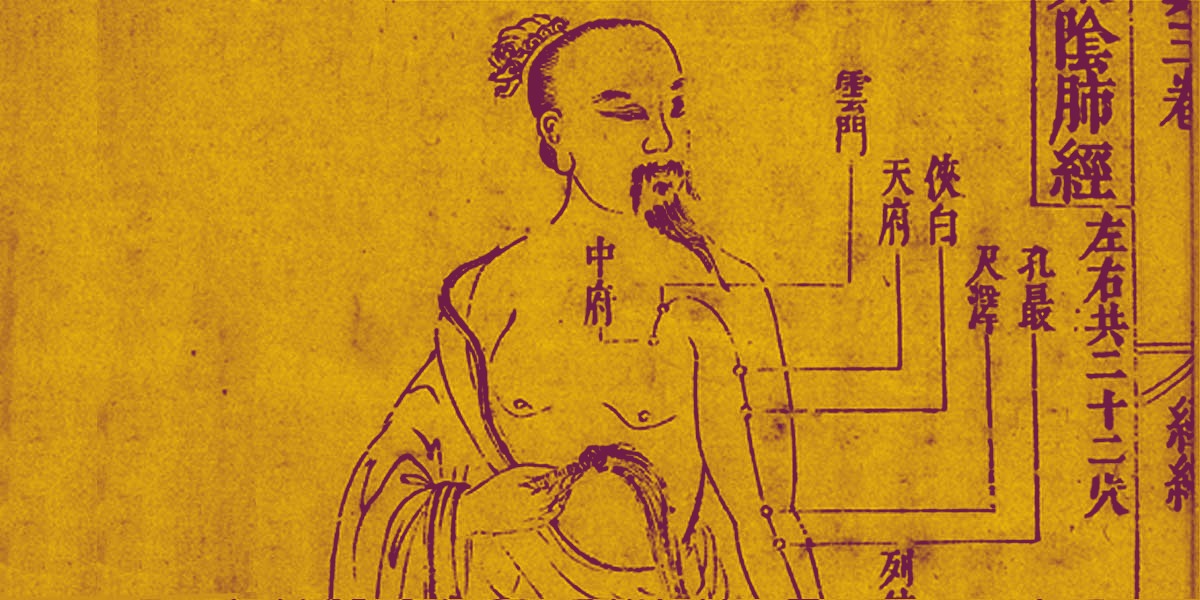
History of Medicine and Medical Humanities Learn More
Through the interdisciplinary field of medical humanities, we learn about the wider historical and cultural content that health care operates in. The History of Medicine and Medical Humanities Research Portal was developed to help gather resources for researchers, health professionals and the general public.
Led by Ellen Amster

MUSIC Learn More
The McMaster University Sentinel and Information Collaboration (MUSIC), is a practice-based research and learning network (PBRLN). MUSIC facilitates high quality research on topics that are important to primary care and the patients it serves.
Led by Michelle Howard

PoET Southwest Spread Project Learn More
Long-term care (LTC) residents are at risk of receiving unwanted and non-beneficial treatment because of errors related to consent. The PoET Southwest Spread Project aims to reduce these consent-related errors and provide care that is in line with the resident’s values and wishes.
Led by Henry Siu

Primary Care in Late Life Learn More
The Primary Care in Late Life research program aims to improve the experience of people with serious and life-limiting illness by studying patterns of health care near the end of life and integrating palliative approaches in primary health care and family medicine.
Led by Michelle Howard

Prison Health Learn More
Our research work in prison health is aimed at preventing incarceration, improving health care in prisons and supporting the continuity of health care on release. Our work in this area involves partnership, collaboration, and consultation with persons with lived experience of incarceration, and other stakeholders and researchers.
Led by Fiona Kouyoumdjian

Social and Ethical Complexity in Primary Care Learn More
Our research enhances patient experience and improves the quality of professional life for clinicians by focusing on socially and ethically complex areas of primary care, such as prenatal testing for disability, cannabis consumption in pregnancy, or medical assistance in dying.
Led by Meredith Vanstone

Sustainable Health Systems Learn More
The Department of Family Medicine has partnered with PEACH Health Ontario (Partnerships for Environmental Action by Clinicians and communities for Hospitals/health care facilities) in its efforts to support climate action within the health care system.
Led by Myles Sergeant

Team Approach to Polypharmacy Evaluation and Reduction (TAPER) Learn More
TAPER brings together pharmacists, family doctors and patients to safely reduce the number of medications a person is taking based on the priorities the patient has set for their own health.
Led by Dee Mangin

Vulnerable Individuals in Primary Care (VIP) Research Lab Learn More
The VIP Research Lab aims to improve health by facilitating equitable access and linkage to primary care for vulnerable populations in Canada and internationally. VIP health equity research projects focus on improving inclusion and equity for those with social, economic, and cultural challenges due to income or race and work towards global justice through global health research leadership.
Led by Gina Agarwal

Division of Palliative Care (Research) Learn More
The Division’s main overarching theme of research and quality improvement (QI) excellence will be on primary-level palliative care across different settings of care and its relationship with specialist-level palliative care. The goal is to understand the role of primary-level palliative care in creating health system capacity to equitably address all the palliative needs of a community and population.
Key Contact: Ashlinder Gill
Projects
Information Box Group
The Art of Seeing Learn More
The Art of Seeing™ is a visual literacy program developed by the McMaster University Department of Family Medicine and the McMaster Museum of Art in partnership. The program encourages participants to develop empathetic, holistic, and humanistic thinking, to enhance personal and professional growth. Through evidence-based looking and facilitated discussion, individuals will interact with each other, artworks, and exhibitions to discover how the work of artists reflects and expresses human experience across time and cultures. This analytic and experiential program uses visual art to generate a deeper understanding of oneself and others.
Led by Joyce Zazulak and Nicole Knibb
CO-RIG I: COVID@Home Learn More
The Extended Care in Hamilton project provided clinical pathways to support family physicians to care for patients with mild or moderate COVID-19 and other chronic conditions. The pathways integrate evidence, tools, electronic medical record (EMR) templates, and oxygen monitors to prevent unnecessary hospitalization and detect deterioration early to expedite necessary hospital transfers. The clinic connects regularly with patients in their home with phone calls that monitor symptoms. Evaluation of the pathways’ success resulted in scale up across Ontario in a provincial program now referred to as COVID@Home.
Led by Dee Mangin
CO-RIG II: COPD Exacerbation Pathway Learn More
The Co-RIG II project focuses on patients experiencing acute exacerbations of chronic obstructive pulmonary disease (AECOPD). A clinical care pathway was built by an expert panel of specialist and primary care physicians to help primary care clinicians monitor their AECOPD patients at home. The pathway also provides numerous resources on chronic obstructive pulmonary disease (COPD) for both patients and clinicians to easily access online via Hamilton Family Medicine (HFAM) website.
Led by Dee Mangin
Indigenous Teaching Through Art (ITTA) Learn More
ITTA was a half-day workshop delivered between 2018 and 2020 and co-designed by Indigenous and non-Indigenous members of the department. The team evaluated the impact of the program on participants’ understanding of the history and current realities of Indigenous Peoples in Canada.
Led by Joyce Zazulak and Lorrie Gallant
Niagara Safer Supply Learn More
The Niagara Safer Supply program aims to serve some of the most vulnerable populations in Niagara to curb rising rates of opioid overdoses and overdose deaths. Best practices, knowledge, and capacity building in safer supply will be incorporated and provided to relevant community agencies, along with frontline health, social, and harm reduction workers.
Led by Karl Stobbe and Ryan Chadwick
RIPPLE-C Learn More
People with chronic health conditions rely on regular contact with their primary care team to manage their symptoms, pre-empt future problems and improve their quality of life. However, in many areas of Canada, the COVID-19 pandemic disrupted access to primary care as the focus was placed on assisting the pandemic response and infection control with a temporary shift to mostly virtual visits where possible. RIPPLE-C will use regularly collected patient data and interviews with patients to understand how COVID-19 did or did not impact the management of chronic conditions in different patient groups.
Led by Michelle Howard
