Residency program
We have developed a balanced and innovative program intended to best support you along the way. Our goal is to prepare you, as a residency graduate, to begin comprehensive practice anywhere in Canada.
Your clinical experiences and academic sessions have been specifically designed to ensure the right exposures in a collegial working environment. The resident-preceptor dyad, a foundational component of our program, supports the feedback and opportunities for growth that you’ll require to develop the key competencies of a capable family physician.
We are a dynamic and supportive program — open to feedback and change. As a resident, you will have an important voice in how the program functions. We have taken a careful approach to the expansion and distribution of our program to ensure that regardless of the site you choose, you will experience a consistent approach to a quality education.
At McMaster, innovation is found not only through “what” you learn and do, but also “how” you learn and do. We are committed to providing you with the best possible training. Whether it be a large teaching unit in an urban centre or a practice in a smaller community or rural environment, we offer a wide variety of locations as your Family Medicine home base.
Expandable List
Our Family Medicine Residency Program is dedicated to the development of competent family physicians providing comprehensive, continuous care.
At the core of our program is a family practice that serves as your home base, with a family physician as the primary preceptor for the full two years. This model provides continuity of care, mentorship and education to you, as a resident.
Our residency program is designed to provide flexible postgraduate training to meet your individual needs, recognizing the varying patterns of practice in different family practice settings. Our program is a distributed learning network with the choice of multiple sites which represent separate CaRMS options.
Regardless of your program site, all residents participate in a common curriculum that includes:
- Priority Plus Topics
- Mental Health and Behavioural Science
- InQuiry
- Practice Management
- Procedural Skills
- Residency Practice Based Small Group (PBSG) Learning Program
Our program has a “horizontally integrated” approach to learning to ensure continuity of care for family medicine patients and mental health and behavioural science learning at all sites. This means that as a resident, you return to your home base practice/site at least two half-days per week for clinical care of family medicine patients and for Mental Health and Behavioural Science tutorials.
There are some differences across sites in terms of the structure and organization of the rest of the clinical rotations. Some sites have traditional block rotations with some horizontal experiences and some have adopted an integrated format that weaves together specialty training combined with time in the family medicine clinic.
All residents complete the same rotations, regardless of whether those rotations are delivered in a block or integrated format.
Each block is equivalent to four weeks with a total of 13 blocks each year. At all sites, specialty rotations and exposures have been chosen and developed for their relevance to family medicine.
All residents who are in the program must be able to travel between preceptor practices and hospital-based rotations easily. All residents are encouraged to have their own transportation. Those residents in the Rural Stream are required to have their own transportation.
As a resident in our program, you will complete the following rotations. These are delivered in different formats across the sites, but all residents experience the same common curriculum though these rotations.
PGY1 Core Experiences
- Family Medicine (four blocks)
- Emergency Medicine (two blocks)
- Care of Children (two blocks)
- Care of the Hospitalized Adult (two blocks)
- Women’s Health (two blocks)
- Family Medicine/Academic (one block)
PGY2 Core Experiences
- Family Medicine (four blocks)
- Rural Family Medicine (two blocks)
- Core Medicine/Surgery (two blocks)
- Care of the Elderly (one block)
- Family Medicine/Academic (one block)
PGY2 Electives
- Elective (three blocks)
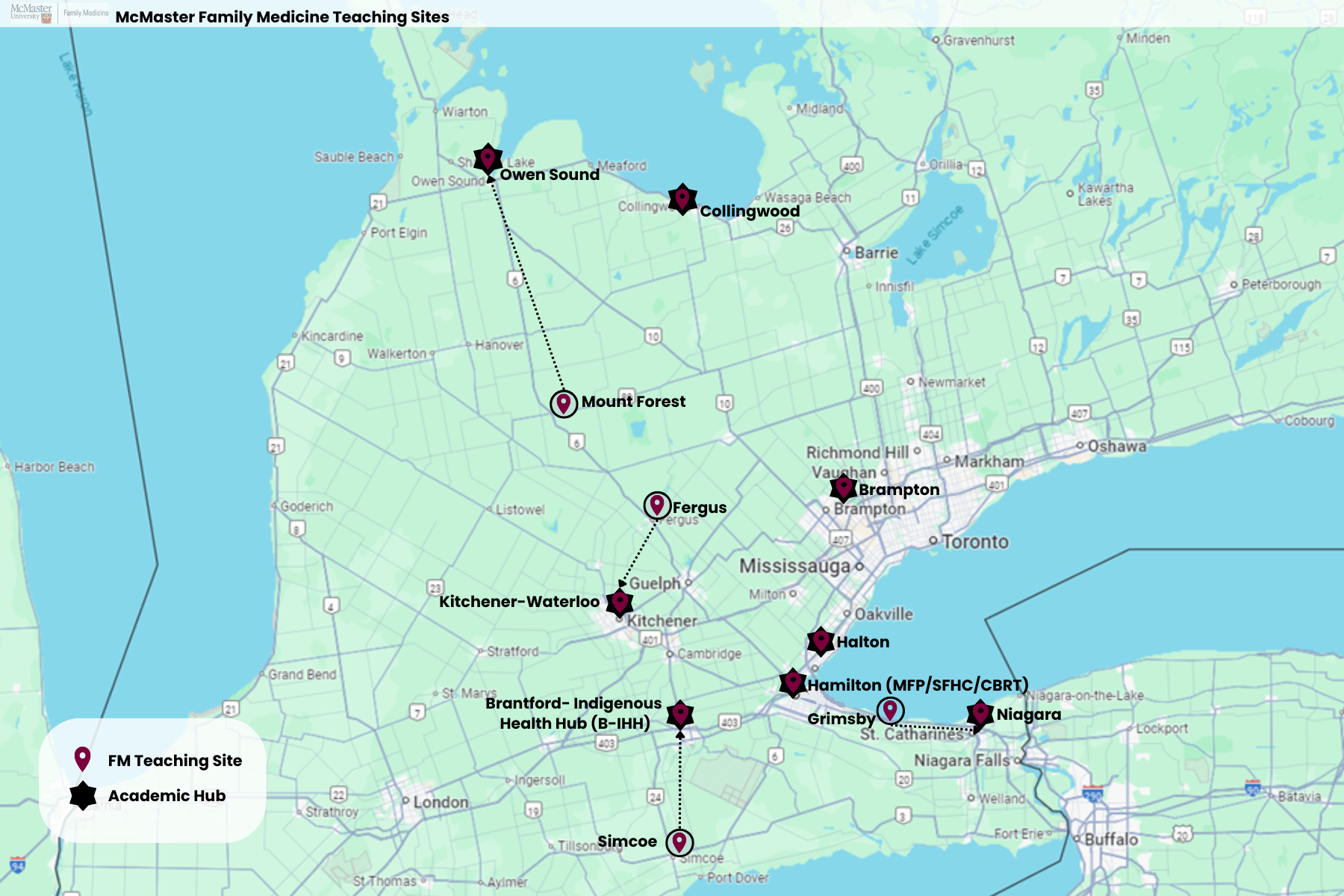
One of the major strengths of our program is the diversity of choices in where you learn and practice as a resident. We offer a choice of seven teaching sites, with our Rural Stream offering a further six community options.
Our sites are spread across southern Ontario and offer a wide range of learning environments. Whatever your clinical or academic interests, and the preferred style of community for you and your family, we have a site that will meet your needs.
Information Box Group
Residency program FAQs - Learn More
How are residents paired with preceptors? Are their specific interests taken into account (e.g. obstetrics, geriatrics)?
Yes! Incoming residents’ interests and preferences are an important factor in matching residents with their primary family medicine preceptors. Although the exact process varies from site to site, it always includes a survey to determine incoming residents’ specific interests and matches them with a preceptor who would be the best fit.
Do residents rotate through other sites or remain with the one they are matched to?
Residents’ core rotations are scheduled at locations within their site. One exception to this is the two-block rural rotation in PGY2 during which we expect residents to travel and experience rural family medicine in another region.
Typically this includes living in that smaller community for the rotation, unless there is a compelling reason that is not possible (such as young children) in which case we ensure a commutable distance.
Residents are certainly invited to pursue opportunities at other sites during elective rotations, and we maintain an electives database to assist in that process.
How many patients do you follow through your “home base practice” as per your continuity of care? And are you expected to be the primary physician for these patients (e.g. calling them to follow up)?
Practice numbers vary from clinic to clinic and the resident list of patients can also vary. The number of patients you see per clinic day will increase as you gain more experience and competency during the program. Ideally, you will follow many of the same patients for continuity during your two-year residency.
Typically, full-time Family Medicine blocks provide the volume required to build a roster of active patients, then during your continuity clinics (half-days back) you will maintain connections with a subset of those patients. We do expect you’ll take on follow up for some of these patients, particularly when you are on full-time family medicine rotation, and when possible during half-days back.
What does a typical call schedule look like? And what kind of supervision is provided?
Family Medicine and off-service rotation call schedules differ from rotation to rotation and site to site, but all adhere to the PARO-CAHO guidelines, All residents are required to participate in a Family Medicine call experience which varies depending on their preceptor’s clinical practice. This may include evening telephone-based call, weekend clinics, urgent care, palliative home-based care and/or long-term care coverage.
Are there any teaching or mentorship opportunities for residents?
Teaching and mentorship are important aspects of medical education and are readily available for interested residents. That said, opportunities may vary from site to site, and are more plentiful at sites connected to the
McMaster Medical Education Campuses –Hamilton, Kitchener-Waterloo, and Niagara.
What are the relationships with off-service residents like? Do FM residents still get prioritized for
procedures, learning opportunities as opposed to more service-based learning?
The number of off-service residents varies from site to site, and from rotation to rotation. You will encounter the most residents from other programs in the Hamilton Site – which affords a robust resident learning community, but also create competition for some opportunities. That said, preceptors are aware of the specific objectives for FM residents, and there are opportunities at all sites to work one-on-one with preceptors in order to maximize procedures, etc. If being the only resident in the hospital, or on rotation is a priority for you, we’d encourage you to look at our smaller urban or rural sites.
How does the clinical experience differ during the rural rotation in second year for those who are matched to a rural site?
Although all Family Medicine residents must complete two-blocks of rural family medicine as part of their program, we realize rural stream-residents already get that exposure through their core family medicine rotations. We use the additional two-block rural rotation in PGY2 to provide a complementary exposure in a different hospital system, often in a more remote or smaller setting, to further develop the skills and competencies required for rural family practice.
Are the rural sites known for having more opportunities to participate in FM OB, surgical assist or hospitalist work?
In addition to Family Medicine clinic, all rural residents have some hospital based experiences embedded throughout the core family medicine rotations. This includes adult inpatient care (MRP) and integrated Emergency Medicine shifts for all rural residents. FM-obstetrics opportunities are strongly supported and encouraged.
What are the opportunities for surgical procedures within the program?
All residents will gain experience with common office-based procedures during their family medicine rotations, which typically include injections, office gynecology, joint injections, minor skin procedures. There are also numerous procedural skills and simulation-based sessions run throughout the program, to offer the opportunity to learn and practice skills in suturing, joint injections, obstetrics and emergency response, and more. Residents seeking additional surgical procedures are encouraged to pursue horizontal and block elective opportunities with that in mind.
What programs exist for resident education? Ex. lectures, journal clubs, practical training skills workshops?
We have a really robust academic curriculum that we encourage you to explore through our website. It includes several longitudinal components, such as Academic Half-Days, tutorials in Mental Health & Behavioural Science, quality improvement and evidence-based medicine. Our residents also participate in the Residency Practice-Based Small Group learning program which use case-based modules to anchor small group facilitated discussion.
In addition to the longitudinal curriculum, we have a number of academic sessions concentrated during block 7 – which falls during the Dec/Jan time frame. These include a mix of didactic sessions, hands-on procedural skills and simulation, skill development workshops and transition to practice sessions.
What are some of the opportunities related to improving research skills? What kind of support do residents
get to complete research projects?
Our program prides itself on our recently integrated InQuiry curriculum, which combines both training in evidence-based medicine as well as quality improvement. This is a mandatory part of the curriculum wherein a QI project is required prior to graduation. Residents are provided protected time and regular check-ins with their IQ tutors to support their QI research during their academic day. For those residents with a more significant research interest, our Research and Scholarship Lead is a valuable mentor and resource who supports connections to faculty, projects and skill development opportunities across the department through electives and more.
What are the global health opportunities?
The global health curriculum not only refers to activities outside of Canada but also transcends borders and
addresses issues of health inequities related to issues of poverty within our own communities. Core competencies related to global health are addressed through our academic curriculum, in Academic Half Day, as well as Mental Health and Behavioural Sciences. There are many clinical opportunities that incorporate care for systemically and historically vulnerable populations across our sites, including shelter health, addictions clinics, care for migrant workers, etc. While some of this work may be embedded in core rotations, it can be supplemented through horizontal and block elective planning. International electives are also available and are noted in the next question below.
Are there any opportunities for international electives?
Residents are welcome to further develop their skills within a global health mindset, placing a priority on improving health and achieving equity in health for all people worldwide. McMaster has a unique partnership with Syiah Kuala University in Aceh, Indonesia to support the development of a medical school curriculum in the areas of disaster preparedness and risk reduction in family medicine. Elective opportunities are available in various areas and are arranged based on residents’ individual interests.
What does the Indigenous Health curriculum look like? Is there any engagement within the community from a clinical and/or cultural aspect?
With support from cultural leaders within the Six Nations community, our Indigenous Health curriculum will assist learners in developing an approach to providing care for Indigenous people that incorporates an understanding of the historical and sociopolitical context of Indigenous people in Canada, honours a Two-Eyed Seeing Approach to providing health care and recognizes the importance of the relationship in all interactions with Indigenous people. Most notably, a longitudinal, integrated Indigenous Health curriculum has been implemented at our Grand Erie Six Nations site and is being expanded program wide.
Are there wellness opportunities or time to connect/socialize with your fellow residents?
Resident well-being is a priority in our program, with dedicated space and support in place throughout a resident’s training. The Mental Health & Behavioural Science program allows for residents to check-in with their small group during tutorial each week, to speak to their experiences on rotation, challenges they may be facing or to share parts of their personal life, to celebrate joys and seek support as needed.
There is also an opportunity for preceptors to connect with residents during the portfolio review, to see how they are doing overall.
Events are planned at both a site and central level with wellness in mind, whether it be allowing for purposeful breaks and lunches, or ensuring there is an opportunity for a fun, social activity to bring the group together.
Read our Residency Program Frequently Asked Questions in PDF format.
Information Box Group

Research Learn More
Interested in research? Discover the opportunities with our research teams.

About DFM Learn More
Check out more information about the Department of Family Medicine at McMaster University.

Latest news from education Learn More
Read the latest news from the education team, residents, educators and more.
Teaching Sites
Urban Sites
Brampton Learn More
Peel Memorial Centre for Integrated Health and Wellness, 20 Lynch Street, Room 2.B.213
Brampton, ON, L6W 2Z8
Brantford-Indigenous Health Hub Learn More
200 Terrace Hill Street
Brantford, ON, N3R 1G9
Halton Learn More
1221 Lakeshore Road
Burlington, ON, L7S 1A7
Hamilton Learn More
100 Main Street West
Hamilton, ON, L8P 1H6
McMaster Family Practice (Hamilton) Learn More
100 Main Street West
Hamilton, ON, L8P 1H6
Stonechurch Family Health Centre (Hamilton) Learn More
1475 Upper Ottawa Street
Hamilton, ON, L8W 3J6
Kitchener-Waterloo Learn More
10B Victoria Street South
Kitchener, ON, N2G 1C5
Niagara Learn More
1812 Sir Isaac Brock Way
St. Catharines, ON, L2S 3A1
Rural Sites
International Medical Graduates
An International Medical Graduate (IMG) is a Canadian citizen or permanent resident who graduates from a medical school outside of Canada.*
*the IMG group includes graduates from American schools of Osteopathic Medicine.
There is a separate admission process for IMGs to Family Medicine Residency, which involves CaRMS, assignment to a cohort group, a pre-residency training program and an assessment verification period. See below for more information on each of these steps.
Resources for IMGs:
- Healthforce Ontario Access Centre – offers services for IMGs who are interested in practicing in Ontario and require counselling
- Ontario IMG School
- Ontario Bridge Training Program
- Touchstone Institute
- CaRMS
- Observerships
- National Assessment Collaboration Examination
Expandable List
The seven Ontario Family Medicine Residency programs jointly run the IMG admissions process via the Canadian Residency Matching Service (CaRMS). Please review the CaRMS website for admission requirements and match timelines.
All IMGs entering Family Medicine Programs in Ontario are required to complete a pre-residency training program (PRP) as a transition to family medicine in Canada. During the PRP, IMGs are treated as fourth-year clinical clerks and have the expectations and responsibilities appropriate for that level. The Pre-Residency Program is divided into two phases:
Pre-Residency Program Phase 1 (PRP1) is organized centrally by Touchstone Institute for all International Medical Graduates commencing Family Medicine Residency Programs in Ontario.
Pre-Residency Program Phase 2 (PRP2) is organized locally for IMGs commencing family medicine at McMaster University by individual teaching sites, with the goal of addressing identified needs of IMGs prior to residency. During this period, participants attend the Academic Half Day at their teaching site.
*Access to a car and ability to drive may be required for pre-residency training as well as throughout residency. Go to the Ontario website for information on how to exchange your out-of-country driver’s license.
In addition to helping IMGs transition to family medicine in Canada, the PRP also prepares IMGs for a successful evaluation in the mandatory Assessment Verification Period.
The College of Physicians and Surgeons of Ontario (CPSO) requires all International Medical Students to complete a 12-week Assessment Verification Process (AVP) following the Pre-Residency Training Program. IMGs must successfully complete the AVP in order to receive a postgraduate educational license to practice medicine in Canada and start residency training.
Enhanced Skills
McMaster University’s Department of Family Medicine offers a robust third-year (PGY-3) Enhanced Skills program for residents interested in pursuing additional training after the core two-year Family Medicine Residency.
With a focus on preparing physicians to be responsive to the needs of individual communities, the Enhanced Skills program provides additional experience and/or advanced training in a range of specific areas.
Program Options
Our Enhanced Skills Program offers a wide range of options that give residents the benefit of additional experiences as they prepare for their future practices. Interested residents in their second year will apply to either Category 1 or Category 2 – Self-Designed programs based on their career intentions.
Category 1 programs are those designated by the CFPC as programs leading to a Certificate of Added Competence. The majority of these programs are offered in Hamilton (FPA excepted), but many offer training opportunities in other urban settings and/or rural/regional contexts.
Category 2 – Self-Designed programs are intended for learners to gain additional experiences in research and scholarship or an individual area of interest, or to enhance skills designed to fill the needs of a rural/regional community. Self-Designed and Category 2 programs do not lead to a Certificate of Added Competence at completion.
The department is committed to promoting flexible Enhanced Skills training options that provide community-in-need focus and allow FM graduates to pursue specialized practice opportunities in rural, remote and regional settings.
Information Box Group
Expandable List
Click the name of each program for full details.
| CATEGORY | PROGRAM | CERTIFICATE OF ADDED COMPETENCE | MONTHS/POSITIONS AVAILABLE | PRIMARY PRACTICE SETTING |
|---|---|---|---|---|
| CATEGORY 1 | Addiction Medicine | Yes | One 12-Month Position | Waterloo Region |
| Care of Elderly | Yes | Two 12-Month Positions | Hamilton (1)
Niagara (1) |
|
| Palliative Care | Yes | Four 12-Month Positions | Hamilton | |
| Sports and Exercise Medicine (SEM) | Yes | One 12-Month Position | Burlington/Hamilton | |
| Emergency Medicine | Yes | Nine 12-Month Positions
|
Hamilton (5) KW (2) Niagara (2) |
|
| Family Practice Anesthesia (FPA) | Yes | Three 12-Month Positions | Rural/Regional/Brantford/Hamilton | |
| CATEGORY 2 | Rural/Regional Self-Designed | No | 3-6 Months (6 to 8 positions) | Rural/Regional |
| Research & Scholarship | No | One 12 Month Position | Hamilton | |
| Family Medicine Obstetrics | No | Two Six-Month Positions | Hamilton |
The department can offer the rural/regional placements through its partnerships with the Rural Ontario Medical Program (ROMP) and Mac-CARE. For further information on Rural/Regional program experiences offered, please see our rural/regional information page.
Information Box Group
Eligibility
All Family Medicine PGY2 learners currently training in Canada, independent of residency location, are eligible to apply for any of our Enhanced Skills programs. The Enhanced Skills Program reviews applications from PGY2 residents who are registered in a Canadian Family Medicine Residency Program at the time of their application.
Residents must start their PGY3 year within 12 months of completing their PGY2 year.
Practicing physicians wishing to apply to the Enhanced Skills Program must do so through the Re-Entry Program offered by the Ministry of Health and Long-Term Care; applications made directly to the university will not be accepted. Please view information about the Re-Entry Program on the Ministry of Health website. Different timelines apply to Re-Entry Applicants.
For International Medical Graduate (IMG) applicants, please review information related to eligibility and Return of Service (ROS) here.
Admissions deadlines
| 2024-2025 Family Medicine/Enhanced Skills Match Timeline (Category 1 & 2 Programs) | |
|---|---|
| July 30, 2024 at 12:00 (noon) ET | Application Opens |
| September 10, 2024 at 12:00 (noon) ET | Applicant document submission deadline |
| October 4, 2024 | Interview status for Category 1 applicants will be updated through CaRMS Online |
| October 11, 2024 – November 29, 2024 | National interview period (Category 1 interview dates published on CaRMS Online, exact interview days by Category 2 program TBD) |
| December 12, 2024 at 12:00 (noon) ET | MATCH DAY – Category 1 Program match, and Category 2 offer letters |
| For more details, please refer to CaRMS. | |
How to apply
Category 1: Applications must be made through CaRMS. Please see the CaRMS website for more information.
Category 2:
- Save and fill out the Category 2 Enhanced Skills Application Form (PDF)
- Submit your completed application, along with your CV and letter of intent to fmpgy3@mcmaster.ca
- Ensure that the subject line of your application email follows this format: “Last name, First name – 20XX/20XX Application” (please indicate the academic year you are applying for).
- Request that your Program/Site Director and two referees send their letters directly to us at fmpgy3@mcmaster.ca. If you have any questions, please contact fmpgy3@mcmaster.ca
Checklist:
- Updated curriculum vitae – including any advanced life support courses and electives
- Completed application form
- Letter of intent, including the following:
- Your goals and objectives for the program
- The ways you might be better enabled to contribute to the community, the Department of Family Medicine, or the discipline of Family Medicine in general
- For applicants to Research/Scholarship only, please describe your experience with research/scholarship thus far; an area of inquiry that interests you; and how developed your scholarly project(s) idea is at this point.
- Letter of Support from your Program Director, which speaks to your academic performance and professionalism*
- Two letters of reference from supervisor(s)*
*Please have reference letters sent directly to the following via mail or email (email preferred):
Department of Family Medicinec/o Shauna Ferguson – Enhanced Skills Application
David Braley Health Sciences Centre
100 Main Street West, 2nd Floor
Hamilton, ON L8P 1H6
OR
Email: fmpgy3@mcmaster.ca
Information Box Group
FAQs
Do I need to have an elective in the field I wish to apply for?
Electives are not required but are strongly encouraged, where possible, to gain exposure and test your interests in a certain area of focus.
I am a practicing physician outside of Canada. Can I apply?
The Ministry of Health and Long Term care will only provide funding for residents and physicians who are either practicing in Canada or completing their residency in Canada
What is the difference between Category 1 and Category 2 – Self-Designed programs?
Category 1 programs lead to a Certificate of Added Competence, as recognized by the CFPC.
If I want to practice in a rural setting afterwards, which programs will support that goal?
Our Self-Designed programs are designed to provide a resident with the skills and experience to support a rural/regional practice. Discussions with your Program Director will help determine which experience will best suit your interests and the needs of the community in which you hope to practice.
For more information, please see our programs page or contact Fmpgy3@mcmaster.ca
Enhanced Skills Information Session View Recording
The 2024 Enhanced Skills Information Session was hosted October 2, 2024.
Enhanced Skills Information Session - View Recording
Contact us
We are here to support you through every step of your ongoing skills enhancement. Please do not hesitate to contact us with any questions or concerns you have.
For the Emergency Medicine Program, contact Kelly Binkle fmemerg@mcmaster.ca
For all other programs, contact fmpgy3@mcmaster.ca.
Contacts
Our Education team is happy to speak with you about our undergraduate and postgraduate programs. We have a large team of staff and faculty dedicated to running these programs.
Review our faculty member and staff directories online to learn more.
Download the contact information for our Enhanced Skills Programs and PG Central Office and Curriculum Coordinators.
Information Box Group
Family Medicine - general inquiries
For general postgraduate inquiries, please contact fm-pg@mcmaster.ca.
Enhanced Skills Program - general inquiries
For general Enhanced Skills Program inquiries, please contact fmpgy3@mcmaster.ca.