About Us
Canadians see a primary care provider at multiple points in life: from well-baby visits to end-of-life planning. A primary care provider could be a family physician, nurse practitioner, or other trained health professional and are generally the first called when people have a health concern.
Research has shown the strongest clinical evidence for improving health outcomes in the population is by strengthening primary care. When people have access to strong primary care, they can address a health concern before it leads to a trip to the hospital. So, not only does primary care keep people healthy, it saves health care dollars.
The David Braley Primary Care Research Collaborative (PCRC) was launched in September 2020 to further advance research to strengthen primary care systems through a $4 million investment — seeded by a $1 million contribution by David Braley. This collaborative is the first of its kind in Canada, with the largest endowment supporting a research collaborative in primary care.
The PCRC is bringing together researchers, clinicians, educators and partners to work on issues that will address the diverse needs of our community. We are focused on:
- Building research capacity throughout primary care
- Developing networks of experts, mentors and trainees
- Contributing new evidence to the field of primary care research
- Sharing and implementing knowledge when and where it is needed
- Influencing policy change to improve the health of our communities
Information Box Group
We’re building capacity Research Supports
Resources for growing your primary care research practice.
We’re leading change Research Programs
Learn more about a few of the ways our collaborative is changing primary care.
We’re creating a network of experts Our Researchers
Learn about some of the experts in our network and their research.
Our Research
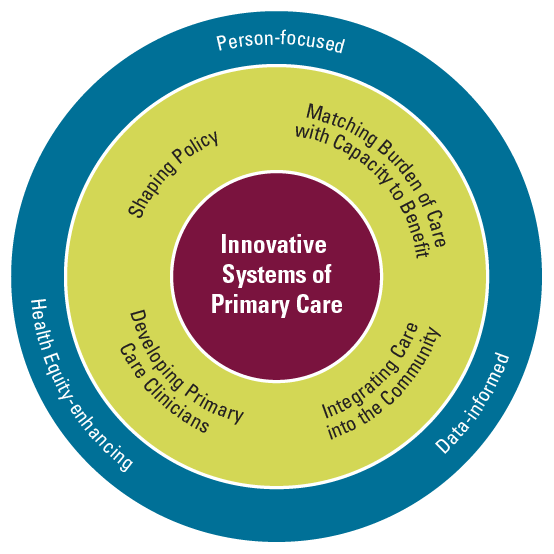
Researchers, clinicians and staff in the department are engaged in practice-based research focused on building innovative systems of primary care using mixed methods, qualitative, and quantitative research designs. The team is working on initiatives to enhance the care that people receive, to improve access to health care particularly for people in greatest need and to change the way the next generation of clinicians are trained.
Information Box Group

We embrace a culture of evidence-informed primary care by working to discover new knowledge and creating new ways to improve the health care patients receive — so that they may enjoy a life worth living on their terms.
Our research, which has informed the development of innovative systems of care and contributed knowledge leading to improved health outcomes, is regularly recognized with local, provincial, national and international awards for excellence.
Information Box Group
$40 million dollars of research funding in the past ten years
Research clusters
Shaping Policy
Policies are an influential element shaping health care delivery. We aim to shape policy through our research and consider the ethical and social implications of health policies to ensure the delivery of sensitive and responsive care.
Developing Primary Care Clinicians
The education and development of clinician trainees is an important part of DFM work and several faculty members are involved in researching how to do this more effectively. Research considers the development of the practicing primary care clinician, drawing attention to how they navigate difficult circumstances, enhance their skillset, and keep up to date.
Integrating Care into the Community across the Lifespan
We have a focus with delivering care to patients where they need it most, which is often in the community. This might mean meeting patients where they are, whether this is elderly people at home, in subsidised housing or in places of incarceration.
Matching Burden of Care with Capacity to Benefit
Established health system practices may not be the best use of resources for patients or for the system. Many of our researchers are considering scenarios that see a potentially high burden of care for a relatively low treatment benefit e.g., overdiagnosis, multimorbidity.
Cross-cutting values
Person-focused
Patient, family, and primary care clinician are the ‘person’ at the centre of the work we do, with particular attention to patient priorities and preferences in clinical care.
Data-informed
Data is important in describing, understanding and shaping practice patterns, the training of clinicians, and identifying places for improving efficiency, efficacy or safety of care.
Health equity-enhancing
Our researchers work to understand and alleviate health inequities experienced by many different types of equity-seeking groups, including racialized and Indigenous populations, gender-diverse and queer populations.
Our Researchers
Researchers at the McMaster University Department of Family Medicine are developing the future of primary care.
Information Box Group
Gina Agarwal
MBBS (UK), PHD (Epidemiology), MRCGP (UK), CCFP, FCFP, Dip. CAPM
Professor
Tier 1 Canada Research Chair in Vulnerable Individuals in Primary Care; McMaster Family Medicine Levitt Scholar; Director, Vulnerable Individuals in Primary Care (VIP) Research Lab; Principal Investigator, McMaster Community Paramedicine Research Team
Dr. Gina Agarwal is a Professor in the Departments of Family Medicine and Health Research Methods, Evidence and Impact and an Associate Professor in the Department of Health and Aging. She is a practicing Family Physician, Primary Care Epidemiologist, the McMaster Family Medicine Levitt Scholar, and the Tier 1 Canada Research Chair in Vulnerable Individuals in Primary Care. She is a member of the McMaster Institute for Research on Aging and the McMaster Institute for Health Equity. Her research achievements have been recognized with the CIHR-IHSPR Article of the Year Award (2019), the prestigious Mid-Career Researcher Award from the North American Primary Care Research Group (2018), and an Award of Excellence from the College of Family Physicians of Canada (2016). As the Director of the Vulnerable Individuals in Primary Care (VIP) Research Lab, she focuses on improving primary health care access for vulnerable populations, ensuring people in need receive appropriate care at the right time and in the right place. As the Principal Investigator of the McMaster Community Paramedicine Research Team, she has driven health system change including the uptake of the innovative Community Paramedicine at Clinic (CP@clinic) program by 51% of Ontario Paramedic Services and its national (e.g. BCEHS) and international (e.g. UK, Australia) scale-up. She has worked extensively in social housing to improve the health of this vulnerable population and identify healthcare usage patterns. Her quantitative and qualitative research, including complex pragmatic studies, uses rigorous methods to produce novel insight into the unmet health needs of traditionally difficult-to-reach populations and determines cost-effective and targeted healthcare solutions nationally and globally. She regularly supervises undergraduate, master’s and doctoral students.
Special Interests: Unmet health needs of vulnerable populations (e.g. social housing residents), Quantitative and qualitative research methods (e.g. community-based RCTs including complex pragmatic studies and cost-effectiveness of community programming), Community Paramedicine, Social Housing, Diabetes, Cost-effective and targeted healthcare solutions, Community programming for the management of chronic health conditions, Low-cost primary care innovations in low and middle-income countries.
VIP Research Lab Website (https://vipresearchlab.ca/)
CP@clinic Website (https://cpatclinic.ca/)

Gina Agarwal
MBBS (UK), PHD (Epidemiology), MRCGP (UK), CCFP, FCFP, Dip. CAPM
Professor
Tier 1 Canada Research Chair in Vulnerable Individuals in Primary Care; McMaster Family Medicine Levitt Scholar; Director, Vulnerable Individuals in Primary Care (VIP) Research Lab; Principal Investigator, McMaster Community Paramedicine Research Team
Ellen Amster
PhD
Associate Professor
Jason A. Hannah Chair in the History of Medicine
Ellen Amster is the Jason A. Hannah Chair in the History of Medicine at McMaster University and Associate Professor in the Departments of Family Medicine and Religious Studies. She received her B.A. from the University of Chicago and Ph.D. from the University of Pennsylvania. Her research engages medicine in France, North America, and the Islamic world, focusing especially on global health, religion and nonwestern healing, women’s histories, and empire. From her award-winning book, Medicine and the Saints: Science, Islam, and the Colonial Encounter in Morocco, 1877-1956 (University of Texas) she developed an interdisciplinary global health field course for undergraduate students and is the Principal Investigator of the Morocco-Canadian Network in Maternal and Infant Health. Ongoing projects include the transnational legacies of race and colonialism in medicine, the history of public health, women and gender in medicine, midwifery, and medical education. Her research has been funded by IIE Fulbright-Hayes, the Chateaubriand Program of the French government, the Social Science Research Council, AIMS, SSHRC, and CIHR. Dr. Amster provides a regular speaker series open to the campus in the history of medicine. Her teaching includes the history of public health, research electives and professional competencies for MD students in the Michael DeGroote School of Medicine, and Islamic and gender studies in the Department of Religious Studies. For everyone to enjoy, she developed the AMS-funded Hannah History of Medicine and Medical Humanities Research Portal, with hundreds of libraries, archives, museums, digital collections, and grants, to browse for research and fun: http://medhumanities.mcmaster.ca.
Special Interests: Maternal and infant health, Islamic bioethics, race and colonialism in medicine, history of medicine, medical education, gender, public health.

Ellen Amster
PhD
Associate Professor
Jason A. Hannah Chair in the History of Medicine
Alison Baker
MSc, MD, CCFP, FCFP
Associate Clinical Professor
Education Assessment Director
Alison Baker is a family physician in Brantford, Ontario, and an Associate Clinical Professor at McMaster University. She teaches medical students and family medicine residents through the Grand Erie Six Nations Clinical Education Campus. She is the Assessment Director and Chair of the Central Competence Committee for McMaster’s Department of Family of Medicine Residency Program. She is a Fellow in the College of Family Physicians of Canada (CFPC) and holds a Clinician Educator Area of Focused Competence from the Royal College of Physicians and Surgeons of Canada. She is the recipient of the DFM 2017 Excellence in Pre-Clerkship teaching award. She is Chair of the CFPC’s Faculty Development Interest Group and Chair of the CFPC’s National Assessment Community of Practice and sits on the College’s Certification Process and Assessment Committee. Her research activities include using simulation to teach essential conversations in palliative care, identifying opportunities for increasing access to palliative care, and examining motivations for pursuing enhanced skill credentials in family medicine. She is the lead physician for the Brant Family Health Organization, medical manager at Avenue Medical Centre, and a member of the strategic planning working group for the Brantford Brant Norfolk Ontario Health Team.

Alison Baker
MSc, MD, CCFP, FCFP
Associate Clinical Professor
Education Assessment Director
Morgan Black
MD
Assistant Professor
Morgan Black is a Family Physician and has been an Assistant Professor with the Department of Family Medicine since 2017. In addition to her work as a Family Physician at McMaster Family Practice, Dr. Black has a significant interest in the domains of Women’s Health and Low Risk Obstetrics. She currently works as a staff physician with the Maternity Centre of Hamilton, providing full prenatal care to vulnerable populations and performing full intrapartum care at St. Joseph’s Healthcare Hamilton. She also has a strong interest in medical education at both a postgraduate and undergraduate level.
Claire Bodkin
Assistant Clinical Professor (Adjunct)

Claire Bodkin
Assistant Clinical Professor (Adjunct)
Keyna Bracken
BSc, MD, CCFP, FCFP
Professor
Chair Pre-Clerkship (UGME)
Keyna Bracken is a Professor in the Department of Family Medicine at McMaster University with a full time academic clinical practice at McMaster Family Practice. The former Undergraduate and Clerkship director for the department of Family Medicine, from 2016 until July 2022, Keyna is now the Chair Pre-Clerkship at the DeGroote School of Medicine where she actively works to champion the discipline of Family Medicine. Keyna is actively involved in teaching both at the undergraduate and postgraduate level with a special clinical interest in Women’s Health which has spanned comprehensive surgical obstetrical care across both high and low resource countries. Keyna has an academic fascination with the topic of optimal clinical learning environments and assessment in undergraduate medical education and is actively involved in several medical education research projects on that topic with both residents and undergraduate learners.
Apart from these scholarly interests and leadership roles, Dr. Bracken enjoys the promotion of Women’s Health care along with the concept of wellness and resilience both nationally and internationally and continues to work toward true reconciliation and the dismantling of the many systems of oppression and racism in both the learning and provision of health care both in Canada and internationally.
Special Interests: Optimal clinical learning environments, promotion of knowledge translation using learning psychology and technology assisted innovation, resilience and wellbeing over the course of medical education.
Martin Chasen
MBChB, FCP(SA), MPhil(Pall Med)
Clinical Professor
Dr. Chasen has been a faculty member of the Department of Family Medicine since 2016. He was born in Pretoria, South Africa, where completed his undergraduate training at the University of Pretoria in 1983, later obtaining a specialist degree in Internal Medicine, Medical Oncology, and Master of Philosophy (Palliative Medicine) at the University of Cape Town.
He is currently the Medical Director of Palliative Care at William Osler Health System in Brampton. He was previously the Medical Director of Palliative Care at The Ottawa Hospital Cancer Centre and the Palliative Rehabilitation Program at Élisabeth Bruyère Ottawa.
Dr. Chasen has over 110 peer-reviewed publications, abstracts, and book chapters. Presently, he is the principal investigator for the RELIEF App study, using digital technology to make palliative care accessible to people in their homes. Dr. Chasen is also involved in the development of European Society for Medical Oncology (ESMO) clinical practice guidelines for patients with anorexia-cachexia and the development of a Pan-Canadian guideline in survivorship. He has led 2 teams to achieve the international ESMO accreditation for Integrated Oncology/Palliative Centres.
Dr. Chasen has received multiple awards, including the Elizabeth J Latimer Prize in Palliative Care from McMaster University, Kay Blair Community Service Award from William Osler Health System, and Eduardo Bruera Award in Palliative Medicine from the CSPCP.
Outside of academia, Dr. Chasen enjoys spending time with his beautiful wife Pamela, two daughters, and two grandchildren. His enjoyment of arts and theatre is one of many of his passions.
Special Interests: Palliative care, survivorship, cancer cachexia, digital health technology.

Martin Chasen
MBChB, FCP(SA), MPhil(Pall Med)
Clinical Professor
Amie Davis
MD, CCFP, FCFP
Associate Professor
Postgraduate Curriculum Director;
Medical Director, Maternity Centre of Hamilton
Dr. Amie Davis is a family physician in the Department of Family Medicine. For the first half of her career, she practiced community-based comprehensive family medicine which included adult inpatient, obstetrical, palliative and outpatient care. She was also the inaugural site director for the Halton Postgraduate Family Medicine residency site. Her work in medical education has allowed her to contribute in the roles of Site Director at many of the McMaster sites including Halton, Niagara and Hamilton. She is currently the Curriculum Director in the postgraduate Family Medicine program with a special interest in entrustment, competency-based learning and curriculum design. She became a full-time faculty member in 2019, and her family practice is located at Stonechurch Family Health centre where her special interests include delivering and teaching gender-affirming primary care, obstetrical care and women’s health. She is the current medical director of the Maternity Centre of Hamilton, where she participates in the collaborative model of expert family medicine obstetrical providers who provide antepartum, intrapartum and postpartum care to pregnant patients with a special expertise in providing care for pregnant people who may be socially at risk.
Special Interests: Family Medicine Obstetrical Care, Gender Affirming Primary Care, Medical Education.

Amie Davis
MD, CCFP, FCFP
Associate Professor
Postgraduate Curriculum Director;
Medical Director, Maternity Centre of Hamilton
Erin Gallagher
BHSc, MD, CCFP (PC), MPH
Associate Professor
Dr. Erin Gallagher is a graduate of McMaster University’s Family Medicine residency program (2015), PGY3 Enhanced Skills Training in Palliative Care program (2016) and Master of Public Health program (2018). In 2017 she completed her Clinical Scholar training through McMaster Family Practice, followed by starting her own general practice in 2017 at Stonechurch Family Health Centre where she trained as a resident.
Through her undergraduate training, Dr. Gallagher discovered her love for medical education and leadership development of medical trainees, the latter being an area of research interest and publication. She is a clinical supervisor and lecturer at the undergraduate and postgraduate levels in the areas of general Family Medicine and Palliative Care. She sits on local, provincial and national committees for Palliative Care education for Family Medicine as well as Medicine and its Subspecialties. Her academic interests include public health approaches to palliative care, including community engagement and development, as well as building capacity for palliative care in primary care.
Clinically, Dr. Gallagher divides her time between providing comprehensive family medicine care to her patients and working as a palliative care consultant for McMaster’s Hamilton teaching sites and Hamilton Health Sciences hospitals. She is the Medical Director at Emmanuel House hospice in Hamilton and the Ontario Health West Physician Clinical Co-Lead for Palliative Care.
Lawrence Grierson
PhD
Associate Professor
Assistant Dean, Health Sciences Education Graduate Program (HSED); Scientist, McMaster Education Research, Innovation, and Theory (MERIT)
Dr. Lawrence Grierson leads research concerned with understanding the relationship between health professions education policies and practices and the quality of healthcare delivered to patients and communities. This work pays specific attention to education antecedents for effective comprehensive family medicine practice, training approaches that promote the acquisition of clinical technical skills, and the ethical inter-institutional collation of training metrics for medical education research.
Dr. Grierson is a member of the Canadian Association of Medical Educators and the CFPC Section of Researchers. He is Associate Professor with the Department of Family Medicine (DFM); Assistant Dean of the Health Sciences Education Graduate Program (HSED); and Scientist with the McMaster FHS Program for Education Research, Innovation, & Theory (MERIT).
Special Interests: Medical and health professions education, admissions and assessment, education research data management, precision technical skills.

Lawrence Grierson
PhD
Associate Professor
Assistant Dean, Health Sciences Education Graduate Program (HSED); Scientist, McMaster Education Research, Innovation, and Theory (MERIT)
Dale Guenter
MD, MPH
Professor Emeritus
Faculty Experience Director
Dale Guenter has experience in community-oriented primary care among populations living on the margins of society and the health system, including people in the inner city, remote northern communities, the Philippines, and people experiencing incarceration. He has been focused clinically on managing illness from blood-born pathogens, chronic pain, addiction and mental health issues. He has pursued teaching, research and program development relevant to all of these areas. The emphasis in all of his work is to learn new ways to be profoundly relationship-centred, equity-seeking, and system-improving. His clinical role is with Shelter Health Network in Hamilton. He works to humanize the experience family medicine faculty members in his role as the Faculty Experience Director.
Michelle Howard
BA (Hons), MSc, PhD
Associate Professor
Michelle Howard is an Associate Professor in the Department of Family Medicine. Her research focuses on understanding the role of primary care for people with serious and life-limiting illness, by examining the influences of practice models, patterns and policies using health administrative and clinical data. She has also studied how patients and health care professionals in primary care talk about serious illness and preparing for future decision-making and has evaluated several tools for advance care planning in family practice.
Michelle has an MSc in Epidemiology from the University of Toronto and a PhD in Health Research Methodology from McMaster University. She primarily uses quantitative approaches including observational studies with population-based data (e.g. www.ices.on.ca www.cpcssn.ca), survey research and development of measures.
Michelle is an instructor for the Program Evaluation course in the McMaster Health Science Education (HSED) program and supervises graduate students with relevant research interests in McMaster’s Health Research Methodology Program.
Gabrielle Inglis
MD, MMSc, CCFP
Assistant Professor (on leave)
Gabrielle Inglis joined the Department of Family Medicine as an Assistant Professor in 2019. In addition to her clinical practice at McMaster Family Practice, she works as a Consultant Physician with the Inpatient Addiction Medicine Service at Hamilton Health Sciences and St. Joseph’s Hospital. Prior to joining the department, she completed a Masters in Medical Education at Harvard University, and is actively involved in post-graduate and undergraduate medical education.
Special Interests: Care for People who use Drugs, Primary care generalism, Medical Education, Narrative Medicine
Fiona Kouyoumdjian
MD, MPH, PhD, FCFP, FRCPC
Research Director & Assistant Professor
Fiona Kouyoumdjian is a Family Physician, Public Health and Preventive Medicine Physician, and Epidemiologist. She received her BA with Honors from Brown University, her MD from Dalhousie University, her MPH from the Johns Hopkins Bloomberg School of Public Health, and her PhD in Epidemiology from the University of Toronto Dalla Lana School of Public Health. She completed residency training at the University of Toronto and a CIHR Fellowship at St. Michael’s Hospital.
Fiona leads a program of research focused on the health status and health care of people who experience imprisonment. Her specific research foci are decreasing imprisonment, improving health care and health promotion for people in prison, and supporting successful re-integration to the community for people on release from prison.
Fiona is also an Adjunct Scientist at ICES and an Associate Member in the Department of Health Research Methods, Evidence, and Impact at McMaster.

Fiona Kouyoumdjian
MD, MPH, PhD, FCFP, FRCPC
Research Director & Assistant Professor
Linda Lee
MD, CCFP(COE), FCFP, MClSc
Associate Clinical Professor
Dr. Linda Lee is a Care of the Elderly family physician, Associate Clinical Professor in the Department of Family Medicine at McMaster University, Director of the Centre for Family Medicine and KW Regional Memory Clinics, and Schlegel Chair in Primary Care for Elders. She has developed the MINT Memory Clinic model and Training Program which has assisted 120 other primary care settings in Ontario, BC, Alberta, and Saskatchewan to establish new MINT Memory Clinics. Dr. Lee’s research interests focus on improving health care for older adults living with dementia and other complex chronic conditions. She enjoys time with family, growing tomatoes, and raising parrots.
Special Interests: community-based dementia care, frailty in primary care.

Linda Lee
MD, CCFP(COE), FCFP, MClSc
Associate Clinical Professor
Robin Lennox
MD, CCFP
Assistant Clinical Professor
Robin Lennox has been a Family Physician and Assistant Professor with the Department of Family Medicine since 2017. She has a clinical focus in the care of people who use drugs, which includes working with the Rapid Access Addiction Medicine Clinic and the Program for Substance Use in Pregnancy at the Maternity Centre of Hamilton. She is co-Head of Service for the Inpatient Addiction Medicine Service at Hamilton Health Sciences and St. Joseph’s Healthcare Hamilton. In addition, Dr. Lennox works with the Shelter Health Network providing primary care for people deprived of housing. She has a diverse research portfolio aimed at improving models of care delivery and the health outcomes of people who use drugs with infectious complications, and improving the experiences of people who use drugs when interacting with the health system.
Special Interests: Care of People Who Use Drugs, Addiction Medicine, HIV primary care, gender diverse care, care of people deprived of housing.
Dee Mangin
MBChB, FRNZCGP, DPH
Professor (Part-Time)
Derelie (Dee) Mangin is a professor in the Department of Family Medicine, where she has held the distinguished David Braley Nancy Gordon Chair since 2013. Her academic interests include the role and value of generalist primary care; innovative models of primary care delivery; rational prescribing; effective incorporation of evidence into patient centered practice; and the influences of science, policy and commerce on the nature of care. An area of current focus is multimorbidity and polypharmacy among older adults as a lens for promoting care that maps onto patient priorities and where the burden or care does not exceed the patient’s capacity to benefit. She has wide clinical research experience in primary care, including observational and interventional quantitative research methods and community randomized control trials (RCTs) of innovative models of care. She is currently director of the McMaster University Sentinel and Information Collaboration (MUSIC) practice based research network. Dee has experience leading RCTs of clinical interventions in areas such as antidepressant use, community acquired pneumonia, antibiotics in urinary tract infections, and deprescription trials. She has received award for leadership in Family Medicine and in Family Medicine research that include the Royal New Zealand College of General Practitioners Distinguished Service Award and the Canadian College of Family Physicians Donald I Rice Award.
Special Interests: The role and value of generalist primary care in the health system; innovative models of primary care delivery; rational prescribing; effective incorporation of evidence into patient centered practice; and the influences of science, policy and commerce on the nature of care.
Anjali Menezes
Assistant Clinical Professor (Adjunct)

Anjali Menezes
Assistant Clinical Professor (Adjunct)
James Milligan
BSc.P.T., MD, CCFP, FCFP
Assistant Clinical Professor
Family physician with the Centre for Family Medicine (CFFM) Kitchener-Waterloo. Director of the CFFM Mobility Clinic, an interprofessional primary care clinic with a focus to improve primary care for individuals with spinal cord injury and other physical disabilities. The clinic is dedicated to clinical research in primary care, working closely with the Praxis Spinal Cord Injury Institute. Associate Clinical Professor with the McMaster University Department of Family Medicine and Clinical Specialist for Mobility and Falls with the University of Waterloo-Schlegel Research Institute for Aging (UW-RIA).
Special Interests: Director Mobility Clinic. Interest in primary care research involving spinal cord injury and physical disabilities.
Margo Mountjoy
MD, PhD, CCFP(SEM), FCFP, FACSM, Dip Sport Med.
Clinical Professor
Dr. Mountjoy is a Clinical Professor in the Department of Family Medicine at McMaster University Medical School and Regional Assistant Dean of the Michael G. DeGroote School of Medicine, McMaster University. She is also a clinician scientist – working for several International Sports organizations in the field of sports medicine including the International Olympic Committee (Games Group), the Association of Summer Olympic International Federations, FIFA, International Golf Federation, World Rugby, and for the World Anti-Doping Agency. She is a retired elite synchronized swimmer. One of her areas of expertise is in the field of harassment + abuse in sport, athlete mental health and female athlete health She is an active advocate of athlete health and well-being at the national and international levels.
Special Interests: Sport and exercise medicine, medical education.

Margo Mountjoy
MD, PhD, CCFP(SEM), FCFP, FACSM, Dip Sport Med.
Clinical Professor
Danielle O'Toole
MD, CCFP
Associate Professor

Danielle O'Toole
MD, CCFP
Associate Professor
Doug Oliver
BSc, MSc, MD, CCFP
Associate Professor
Medical Director, McMaster Family Practice
Dr. Oliver is an Associate Professor in the Department of Family Medicine at McMaster University.
He joined the Department in 2004 and took on a full-time faculty position in 2007.
Dr. Oliver’s passion for elder care lead him to take on the position as Care of the Elderly Curriculum Coordinator from 2006 – 2015. This role allowed him to develop many innovative programs for the Department, including a Long Term Care clinical rotation for residents and a successful annual CME event entitled “Care of the Elderly: Perspectives for Primary Care”. His clinical commitment to this patient population continues with weekly nursing home rounds and house-calls to frail elderly patients.
He is also co-PI on Health Tapestry, a multi-year, multi-site primary care based intervention aimed at promoting optimal aging in community dwelling older adults. Dr. Oliver’s interest in improving access for patients in primary care resulted in study and co-development of an Advanced Access booking model in the McMaster Family Health Team. This model allows patients better access to their primary care team by having the majority of booking spots available for same day appointments.
Dr. Oliver is the Principle Investigator on a research project designed to better understand how and why patients make the choices they do, when calling in to book an appointment with their family doctor. On the academic front, Dr. Oliver is assisting the Department with several educational leadership roles including Co-Education Coordinator at McMaster Family Practice (2011-16), Hamilton Site Director and CBRT Education Coordinator (2012-2013) and Behavioural Sciences Co-Coordinator (2013-).
Dr. Oliver has held several academic leadership roles in the last few years, including Education Coordinator at MFP (2011-16), MHBS Curriculum Coordinator (2013-2019) and is currently the Medical Director at McMaster Family Practice (2016-present)”

Doug Oliver
BSc, MSc, MD, CCFP
Associate Professor
Medical Director, McMaster Family Practice
David Price
BSc, MD, CCFP, FCFP
Professor
Dr. David Price – Professor and Past-Chair (2006-2021), Department of Family Medicine at McMaster University. During his tenure as chair, the Department grew exponentially, graduating over 100 family medicine residents annually in what is generally acknowledged to be one of the top academic programs in the country. As part of the residency expansion; teaching units and/or Family Health Teams (FHT) were created in a number of communities in south central Ontario. Department owned and managed teaching sites include Burlington, Stonechurch and MFP. He was the founding director of the Maternity Centre of Hamilton; a multidisciplinary centre that cares for prenatal and intrapartum patients. Dr. Price was also instrumental in helping to create the academic FHT at McMaster University, an interprofessional team, currently serving over 40,000 patients in the Hamilton area. He was a key player in the development of the $85 M, David Braley Health Sciences Centre, a six-story, 185,000 sq. ft. home for Family Medicine and Hamilton Public Health in the downtown core. The research enterprise of the department has also grown in size and reputation, managing over $10M in research grants annually. He also led the creation of a second endowed chair in family medicine ($2 million), the Niagara professorship ($1 million) and the establishment of the David Braley Primary Care Research Collaborative with an additional $4 million endowment.
Through his leadership roles at the University and Hospital (Chief of Family Medicine at Hamilton Health Sciences from 2004-2018), and his involvement with local, regional, and provincial government bodies where he acts as a consultant and advisor, he has developed expertise in primary care reform and health care policy development. He has provided his expertise to provincial governments in Canada, as well as internationally. He has enjoyed learning about other primary care systems around the world during his many visits as an invited speaker to numerous countries.
As the Chair of the Provincial (Ontario) Expert Advisory Panel on Primary Care (2013-2014) he was instrumental in helping produce “Patient Care Groups: A new model of population based primary health care for Ontario” (“Price Report”). He is currently the chair of the Minister of Health’s Primary Care Advisory Table, and has been on Ontario’s Covid-19 Health Coordination Table since April 2020. At the University, he is chair of the Faculty of Health Sciences Finance Committee, and as Secretary of Regional Medical Associates, the incoming president (fall 2022). In July 2021, he became the co-lead of the Health Leadership Academy (a partnership between the DeGroote School of Medicine and DeGroote School of Business).
Amanda Ramdyal
MD, CCFP, MSc
Assistant Professor
Education Coordinator
Dr. Amanda Ramdyal is Family Physician and joined the Department of Family Medicine in 2016 as a locum, and then became an Assistant Professor in 2017. She has a strong clinical interest in women’s health and sexual health. Dr. Ramdyal is a staff physician at Stonechurch Family Health Centre, as well as with Hamilton Public Health Sexual Health Clinic. She has a special research interest in prevention, screening and management of sexually transmitted infections.

Amanda Ramdyal
MD, CCFP, MSc
Assistant Professor
Education Coordinator
Lynda Redwood-Campbell
MD, FCFP, MPH
Professor
Dr. Redwood-Campbell is a full-time faculty member and Full Professor in the Department of Family Medicine since 1996. She is the co-director, Global Health for Postgraduate Medical Education McMaster University. She has a keen interest and expertise in Global Health. She completed her MD and residency at McMaster and her Diploma in Hygiene and Public Health in London UK at the London School of Tropical Medicine and Hygiene. She additionally completed her Master’s in Public Health at Johns Hopkins Bloomberg School of Public Health. She has been involved in global health partnerships in primary care and global family medicine. She is the current Chair, Besrour Global Family Medicine Advisory Council. She has decades of experience international disaster humanitarian work mostly with the Canadian and International Red Cross. She has worked in many countries like Indonesia, Bangladesh, the Philippines, Haiti, Mozambique, Nepal and more. She is the recipient of the OMA Presidential Award, which recognizes long-standing humanitarian service to the greater community. Her more recent research focused on lessons learned by healthcare teams doing international humanitarian work and how this is directly applicable to the Canadian context. In 2023, she is a member of the Ontario Public Health Emergencies Science Advisory Council. She enjoys teaching medical residents and students in a broad family medicine context. Dr. Redwood-Campbell has a clinical practice at McMaster University and enjoys the Canadian outdoors. Further information can be found at https://mcmasterfamilypractice.ca/bios/lynda-redwood-campbell/
Special Interests: Global Health, humanitarian response, complex humanitarian emergencies, immigrant and refugee health, primary health care, global family medicine, equity in healthcare, medical education, teaching in medicine, quality assurance.
Cathy Risdon
MD, DMan, CCFP, FCFP
Professor & Chair
Dr. Cathy Risdon is Professor and Chair of the Department of Family Medicine at McMaster aiming to help reinvigorate a sustainable, inclusive learning and practice environment for current and future family medicine learners and providers. For Risdon, breaking down barriers and honouring different viewpoints is key to building a successful department capable of training top-quality family doctors and attracting skilled staff and faculty.
She was the first holder of the David Braley-Nancy Gordon Endowed Chair in Family Medicine, mandated to develop innovations in education, clinical service and research relating to the doctor-patient and interdisciplinary team relationships. She co-created the Michael G. DeGroote School of Medicine’s Professional Competency Curriculum, a two-year course to teach professionalism, communication skills, advocacy, ethics and reflective practice. Following the ten-year term of her Endowed Chair, she became Associate Chair, Academic within the Department of Family Medicine, as well as the co-lead for the McMaster Family Health Team.
Dr. Risdon has completed a Doctorate of Management in Organizational Change at the University of Hertfordshire where her research explored themes of excellence and improvisation within curriculum design and implementation. She has conducted training and consultations across North America for primary care and community-based agencies wishing to improve their capacity for effective team and interprofessional collaborations. Her expertise in facilitation was used to design and deliver on the successful Hamilton Health Team submission. She is an expert in health system integration and primary care and is one of three Canadians who has been inducted as a Fellow of the Academy of Communications in Healthcare in recognition of her contributions to curricular design and facilitation.
A McMaster graduate (class of ’92), Dr. Risdon’s clinical practice has included a varied inner-city population with a focus on vulnerable populations.
After more than 30 years in the Department of Family Medicine at McMaster, Dr. Risdon is still amazed at her good fortune in working with such terrific people. “We have extraordinary people engaged in our mission of service, teaching, and discovery. It’s my privilege to do all that I can to help them thrive.”
Inge Schabort
MBChB, BScMedScHons (Epi), BScMedScHons (Med Biochem), MSc(EBHC), MHPE, CCFP, FCFP
Associate Professor, Full-time Academic Family Physician, Postgraduate IMG Director
Dr. Inge Schabort is an Associate Professor of Family Medicine and the Postgraduate International Medical Graduate (IMG) Director at the Department of Family Medicine, McMaster University. She practices as a full-time academic family physician at Stonechurch Family Health Centre and she tutors Evidence-Based Medicine, Quality Improvement and Mental Health and Behavioural Sciences in the residency program She just completed her term as Academic Half Day Coordinator in the Department.
Dr Schabort recently completed a Master of Health Professions Education (MHPE) at the University of Maastricht in the Netherlands (2020) and an MSc in Evidence Based Health Care from Oxford University in the UK (2022).
After medical school she worked as a physician in Sub-Saharan Africa for 10 years and completed postgraduate training in obstetrics and gynecology, internal medicine, epidemiology, immunology, endocrinology, biochemistry and pathology before she was recruited to Canada. In Canada it took several years for her to compete for an IMG position in Ontario and then repeat her clerkship as well as complete a family medicine residency in the Ontario IMG program.
Dr. Schabort is an author of the national Future of Medical Education in Canada (FMEC) IMG Environmental Scan document, and she also was a physician-stakeholder consultant for the Pan-Canadian Framework for the Assessment and recognition of foreign qualifications for the entry to Residency pathway. She sat on the Thomson IMG Working Group of the Council of Ontario Universities and is currently representing the CFPC on the national N4 Working Group to leverage IMGs to close healthcare labour market gaps. She completed a comprehensive review of the medical student and resident selection and IMG literature and has published research on IMG selection predictors for success. Her MHPE thesis studied IMG selection in Canada and her Oxford dissertation studied IMGs internationally. She recently completed a systematic review of prognostic studies on predictors for success in IMGs in postgraduate training and practice internationally as part of her Oxford dissertation. She currently sits on the Board of Directors of the Canadian Residency Matching Service as an expert in IMG matters.
Dr. Schabort was on the Ontario Steering Committee for the development of the Curriculum for the Ontario International Medical Graduate Pre-Residency program and currently is on the Curricular Advisory Committee for the Pre-residency IMG program for all RCPSC and CFPC IMGs entering residency training in Ontario. She sat on the provincial steering committee for the development of the curriculum and selection process for Practice Ready Assessment. She sat on the Steering Committee for the Ontario Inter-professional Spinal Assessment Education Clinics (ISAEC) and was the Hamilton Primary Care Lead for the implementation of the ISAEC pilot.
She has authored papers on several topics in medical education and primary care research, and an invited book chapter on International Medical Graduates. She has received several awards including the 2012 Award of Excellence from the College of Family Physicians of Canada and the Glenn Sawyer Service Award from the Ontario Medical Association in 2015 as well as the Professional Association of Residents of Ontario (PARO) Excellence in Clinical Teaching Award in 2021
Her clinical and academic interests include medical education, selection, assessment, remediation, leadership, mentorship, IMG education and advocacy, disease screening, prevention and health promotion global health, inter-professional care and education, vulnerable population health, women’s health, chronic disease management, evidence-based medicine and primary care research.

Inge Schabort
MBChB, BScMedScHons (Epi), BScMedScHons (Med Biochem), MSc(EBHC), MHPE, CCFP, FCFP
Associate Professor, Full-time Academic Family Physician, Postgraduate IMG Director
Henry Siu
MSc, MD, CCFP (COE), FCFP
Associate Professor
Medical Director, Stonechurch Family Health Centre
Henry Siu completed his undergraduate medical training at the University of Toronto in 2008, and his residency training at McMaster University in 2010. He joined the department full time in 2013 and was promoted to the rank of Associate Professor in 2020.
His clinical interests include care of the elderly, especially those living in long-term care. He currently practices at Stonechurch Family Health Centre, and as an attending physician at a local long-term care home.
His current research endeavours involve research in long-term care including auditing advance care planning rates and assessing clinicians barriers to long-term care, implementing a new periodic health examination form, and implementing a tool to support informed consent and alignment of practices in LTC to the Ontario Health Care Consent Act. He has recently received funding from the Canadian Frailty Network and Health Canada to pursue his research interests and have published articles in various journals about his work in long-term care.
Special Interests: Care of the Elderly, Long-term care

Henry Siu
MSc, MD, CCFP (COE), FCFP
Associate Professor
Medical Director, Stonechurch Family Health Centre
Meredith Vanstone
PhD
Associate Professor; Canada Research Chair (Tier 2) in Ethical Complexity in Primary Care
Meredith is an Associate Professor in the Department of Family Medicine and Canada Research Chair (Tier 2) in Ethical Complexity in Primary Care. She uses qualitative approaches to examine social and ethical issues related to health professional practice, education and health policy. In particular, Meredith studies how patients and primary care providers navigate socially and ethically complex care together. Socially or ethically complex care occurs in various places in primary care and Meredith has focused much of her research on complexity related to reproduction, birth, and the end of life. This work has been funded by the Canadian Institutes of Health Research, Public Health Agency of Canada, College of Family Physicians of Canada, and the Greenwall Foundation.
Meredith has a PhD in Health Professional Education from Western University, and has completed postdoctoral studies in Health Policy at McMaster University. She has provided social and ethics evidence and consulting to provincial, national, and international health policy decision-makers.
Meredith supervises graduate students with relevant research interests in the following McMaster graduate programs: Health Policy (PhD), Health Research Methodology (MSc, PhD), Health Science Education (MHSEd).

Meredith Vanstone
PhD
Associate Professor; Canada Research Chair (Tier 2) in Ethical Complexity in Primary Care
Heather Waters
BPE, MD, CCFP, FCFP
Associate Professor
Postgraduate Program Director
Dr. Heather Waters is an Associate Professor in the Department of Family Medicine at McMaster University and has been with the Department since 2000.
Dr. Waters is the Postgraduate Program Director, responsible for leading McMaster’s Family Medicine Residency Training Program across its distributed network of sites. She previously provided educational leadership in Family Medicine in the roles of Hamilton Site Director and Education Coordinator (Stonechurch Family Health Centre).
Dr. Waters works closely with program and CFPC leads in curriculum renewal through the Outcomes of Training Project (OTP). As a member of the CFPC’s Postgraduate Education Committee (PGEC), she contributes to the development of resources to support Family Medicine programs and program directors.
Dr. Waters was McMaster’s former PGME Director of Academic Performance Support and Chair of the Education Advisory Board. In these roles she provided consultation and support to residency programs, program directors, and residents in situation of learner academic difficulty and remediation. She was a founding member of the National Collaboration of Remediation Leads in 2021.
As a member of the Section of Medicine Professionalism Committee and the Professionalism in Practice Working Group at McMaster, Dr. Waters contributes to the development of tools and processes to support professionalism development for learners and faculty. As a member of the CanMeds2025 Expert Working Group on the Professional role, she is contributing to updated postgraduate competency expectations related to professionalism and professional identity formation.
Dr. Waters has a keen interest in medical education and scholarship, particularly related to postgraduate training, generalism and family medicine, professionalism and professional identity formation, humanism and the humanities in medicine, physician and resident wellness, physician leadership, and academic performance support/remediation. She is a member of McMaster’s Education Research, Innovation and Theory (MERIT) Program.
Dr. Waters has had longstanding involvement with the Foundation for Medical Practice Education and the Practice-based Small Group Learning Program (PBSG) as a board member, co-editor, author, peer and resident group facilitator.
As an expert generalist and member of the McMaster Family Health Team, Dr. Waters is actively involved in inter-professional team-based practice and education at Stonechurch Family Health Centre. She provided low risk obstetrical care through the Maternity Centre of Hamilton for twenty years, specializing in care to systemically marginalized women and their families.

Heather Waters
BPE, MD, CCFP, FCFP
Associate Professor
Postgraduate Program Director
Gina Agarwal
MBBS (UK), PHD (Epidemiology), MRCGP (UK), CCFP, FCFP, Dip. CAPM
Professor
Tier 1 Canada Research Chair in Vulnerable Individuals in Primary Care; McMaster Family Medicine Levitt Scholar; Director, Vulnerable Individuals in Primary Care (VIP) Research Lab; Principal Investigator, McMaster Community Paramedicine Research Team
Dr. Gina Agarwal is a Professor in the Departments of Family Medicine and Health Research Methods, Evidence and Impact and an Associate Professor in the Department of Health and Aging. She is a practicing Family Physician, Primary Care Epidemiologist, the McMaster Family Medicine Levitt Scholar, and the Tier 1 Canada Research Chair in Vulnerable Individuals in Primary Care. She is a member of the McMaster Institute for Research on Aging and the McMaster Institute for Health Equity. Her research achievements have been recognized with the CIHR-IHSPR Article of the Year Award (2019), the prestigious Mid-Career Researcher Award from the North American Primary Care Research Group (2018), and an Award of Excellence from the College of Family Physicians of Canada (2016). As the Director of the Vulnerable Individuals in Primary Care (VIP) Research Lab, she focuses on improving primary health care access for vulnerable populations, ensuring people in need receive appropriate care at the right time and in the right place. As the Principal Investigator of the McMaster Community Paramedicine Research Team, she has driven health system change including the uptake of the innovative Community Paramedicine at Clinic (CP@clinic) program by 51% of Ontario Paramedic Services and its national (e.g. BCEHS) and international (e.g. UK, Australia) scale-up. She has worked extensively in social housing to improve the health of this vulnerable population and identify healthcare usage patterns. Her quantitative and qualitative research, including complex pragmatic studies, uses rigorous methods to produce novel insight into the unmet health needs of traditionally difficult-to-reach populations and determines cost-effective and targeted healthcare solutions nationally and globally. She regularly supervises undergraduate, master’s and doctoral students.
Special Interests: Unmet health needs of vulnerable populations (e.g. social housing residents), Quantitative and qualitative research methods (e.g. community-based RCTs including complex pragmatic studies and cost-effectiveness of community programming), Community Paramedicine, Social Housing, Diabetes, Cost-effective and targeted healthcare solutions, Community programming for the management of chronic health conditions, Low-cost primary care innovations in low and middle-income countries.
VIP Research Lab Website (https://vipresearchlab.ca/)
CP@clinic Website (https://cpatclinic.ca/)
Gina Agarwal
MBBS (UK), PHD (Epidemiology), MRCGP (UK), CCFP, FCFP, Dip. CAPM
Professor
Tier 1 Canada Research Chair in Vulnerable Individuals in Primary Care; McMaster Family Medicine Levitt Scholar; Director, Vulnerable Individuals in Primary Care (VIP) Research Lab; Principal Investigator, McMaster Community Paramedicine Research Team
Dr. Gina Agarwal is a Professor in the Departments of Family Medicine and Health Research Methods, Evidence and Impact and an Associate Professor in the Department of Health and Aging. She is a practicing Family Physician, Primary Care Epidemiologist, the McMaster Family Medicine Levitt Scholar, and the Tier 1 Canada Research Chair in Vulnerable Individuals in Primary Care. She is a member of the McMaster Institute for Research on Aging and the McMaster Institute for Health Equity. Her research achievements have been recognized with the CIHR-IHSPR Article of the Year Award (2019), the prestigious Mid-Career Researcher Award from the North American Primary Care Research Group (2018), and an Award of Excellence from the College of Family Physicians of Canada (2016). As the Director of the Vulnerable Individuals in Primary Care (VIP) Research Lab, she focuses on improving primary health care access for vulnerable populations, ensuring people in need receive appropriate care at the right time and in the right place. As the Principal Investigator of the McMaster Community Paramedicine Research Team, she has driven health system change including the uptake of the innovative Community Paramedicine at Clinic (CP@clinic) program by 51% of Ontario Paramedic Services and its national (e.g. BCEHS) and international (e.g. UK, Australia) scale-up. She has worked extensively in social housing to improve the health of this vulnerable population and identify healthcare usage patterns. Her quantitative and qualitative research, including complex pragmatic studies, uses rigorous methods to produce novel insight into the unmet health needs of traditionally difficult-to-reach populations and determines cost-effective and targeted healthcare solutions nationally and globally. She regularly supervises undergraduate, master’s and doctoral students.
Special Interests: Unmet health needs of vulnerable populations (e.g. social housing residents), Quantitative and qualitative research methods (e.g. community-based RCTs including complex pragmatic studies and cost-effectiveness of community programming), Community Paramedicine, Social Housing, Diabetes, Cost-effective and targeted healthcare solutions, Community programming for the management of chronic health conditions, Low-cost primary care innovations in low and middle-income countries.
VIP Research Lab Website (https://vipresearchlab.ca/)
CP@clinic Website (https://cpatclinic.ca/)
Ellen Amster
PhD
Associate Professor
Jason A. Hannah Chair in the History of Medicine
Ellen Amster is the Jason A. Hannah Chair in the History of Medicine at McMaster University and Associate Professor in the Departments of Family Medicine and Religious Studies. She received her B.A. from the University of Chicago and Ph.D. from the University of Pennsylvania. Her research engages medicine in France, North America, and the Islamic world, focusing especially on global health, religion and nonwestern healing, women’s histories, and empire. From her award-winning book, Medicine and the Saints: Science, Islam, and the Colonial Encounter in Morocco, 1877-1956 (University of Texas) she developed an interdisciplinary global health field course for undergraduate students and is the Principal Investigator of the Morocco-Canadian Network in Maternal and Infant Health. Ongoing projects include the transnational legacies of race and colonialism in medicine, the history of public health, women and gender in medicine, midwifery, and medical education. Her research has been funded by IIE Fulbright-Hayes, the Chateaubriand Program of the French government, the Social Science Research Council, AIMS, SSHRC, and CIHR. Dr. Amster provides a regular speaker series open to the campus in the history of medicine. Her teaching includes the history of public health, research electives and professional competencies for MD students in the Michael DeGroote School of Medicine, and Islamic and gender studies in the Department of Religious Studies. For everyone to enjoy, she developed the AMS-funded Hannah History of Medicine and Medical Humanities Research Portal, with hundreds of libraries, archives, museums, digital collections, and grants, to browse for research and fun: http://medhumanities.mcmaster.ca.
Special Interests: Maternal and infant health, Islamic bioethics, race and colonialism in medicine, history of medicine, medical education, gender, public health.
Ellen Amster
PhD
Associate Professor
Jason A. Hannah Chair in the History of Medicine
Ellen Amster is the Jason A. Hannah Chair in the History of Medicine at McMaster University and Associate Professor in the Departments of Family Medicine and Religious Studies. She received her B.A. from the University of Chicago and Ph.D. from the University of Pennsylvania. Her research engages medicine in France, North America, and the Islamic world, focusing especially on global health, religion and nonwestern healing, women’s histories, and empire. From her award-winning book, Medicine and the Saints: Science, Islam, and the Colonial Encounter in Morocco, 1877-1956 (University of Texas) she developed an interdisciplinary global health field course for undergraduate students and is the Principal Investigator of the Morocco-Canadian Network in Maternal and Infant Health. Ongoing projects include the transnational legacies of race and colonialism in medicine, the history of public health, women and gender in medicine, midwifery, and medical education. Her research has been funded by IIE Fulbright-Hayes, the Chateaubriand Program of the French government, the Social Science Research Council, AIMS, SSHRC, and CIHR. Dr. Amster provides a regular speaker series open to the campus in the history of medicine. Her teaching includes the history of public health, research electives and professional competencies for MD students in the Michael DeGroote School of Medicine, and Islamic and gender studies in the Department of Religious Studies. For everyone to enjoy, she developed the AMS-funded Hannah History of Medicine and Medical Humanities Research Portal, with hundreds of libraries, archives, museums, digital collections, and grants, to browse for research and fun: http://medhumanities.mcmaster.ca.
Special Interests: Maternal and infant health, Islamic bioethics, race and colonialism in medicine, history of medicine, medical education, gender, public health.
Alison Baker
MSc, MD, CCFP, FCFP
Associate Clinical Professor
Education Assessment Director
Alison Baker is a family physician in Brantford, Ontario, and an Associate Clinical Professor at McMaster University. She teaches medical students and family medicine residents through the Grand Erie Six Nations Clinical Education Campus. She is the Assessment Director and Chair of the Central Competence Committee for McMaster’s Department of Family of Medicine Residency Program. She is a Fellow in the College of Family Physicians of Canada (CFPC) and holds a Clinician Educator Area of Focused Competence from the Royal College of Physicians and Surgeons of Canada. She is the recipient of the DFM 2017 Excellence in Pre-Clerkship teaching award. She is Chair of the CFPC’s Faculty Development Interest Group and Chair of the CFPC’s National Assessment Community of Practice and sits on the College’s Certification Process and Assessment Committee. Her research activities include using simulation to teach essential conversations in palliative care, identifying opportunities for increasing access to palliative care, and examining motivations for pursuing enhanced skill credentials in family medicine. She is the lead physician for the Brant Family Health Organization, medical manager at Avenue Medical Centre, and a member of the strategic planning working group for the Brantford Brant Norfolk Ontario Health Team.
Alison Baker
MSc, MD, CCFP, FCFP
Associate Clinical Professor
Education Assessment Director
Alison Baker is a family physician in Brantford, Ontario, and an Associate Clinical Professor at McMaster University. She teaches medical students and family medicine residents through the Grand Erie Six Nations Clinical Education Campus. She is the Assessment Director and Chair of the Central Competence Committee for McMaster’s Department of Family of Medicine Residency Program. She is a Fellow in the College of Family Physicians of Canada (CFPC) and holds a Clinician Educator Area of Focused Competence from the Royal College of Physicians and Surgeons of Canada. She is the recipient of the DFM 2017 Excellence in Pre-Clerkship teaching award. She is Chair of the CFPC’s Faculty Development Interest Group and Chair of the CFPC’s National Assessment Community of Practice and sits on the College’s Certification Process and Assessment Committee. Her research activities include using simulation to teach essential conversations in palliative care, identifying opportunities for increasing access to palliative care, and examining motivations for pursuing enhanced skill credentials in family medicine. She is the lead physician for the Brant Family Health Organization, medical manager at Avenue Medical Centre, and a member of the strategic planning working group for the Brantford Brant Norfolk Ontario Health Team.
Morgan Black
MD
Assistant Professor
Morgan Black is a Family Physician and has been an Assistant Professor with the Department of Family Medicine since 2017. In addition to her work as a Family Physician at McMaster Family Practice, Dr. Black has a significant interest in the domains of Women’s Health and Low Risk Obstetrics. She currently works as a staff physician with the Maternity Centre of Hamilton, providing full prenatal care to vulnerable populations and performing full intrapartum care at St. Joseph’s Healthcare Hamilton. She also has a strong interest in medical education at both a postgraduate and undergraduate level.
Morgan Black
MD
Assistant Professor
Morgan Black is a Family Physician and has been an Assistant Professor with the Department of Family Medicine since 2017. In addition to her work as a Family Physician at McMaster Family Practice, Dr. Black has a significant interest in the domains of Women’s Health and Low Risk Obstetrics. She currently works as a staff physician with the Maternity Centre of Hamilton, providing full prenatal care to vulnerable populations and performing full intrapartum care at St. Joseph’s Healthcare Hamilton. She also has a strong interest in medical education at both a postgraduate and undergraduate level.
Claire Bodkin
Assistant Clinical Professor (Adjunct)
Claire Bodkin
Assistant Clinical Professor (Adjunct)
Keyna Bracken
BSc, MD, CCFP, FCFP
Professor
Chair Pre-Clerkship (UGME)
Keyna Bracken is a Professor in the Department of Family Medicine at McMaster University with a full time academic clinical practice at McMaster Family Practice. The former Undergraduate and Clerkship director for the department of Family Medicine, from 2016 until July 2022, Keyna is now the Chair Pre-Clerkship at the DeGroote School of Medicine where she actively works to champion the discipline of Family Medicine. Keyna is actively involved in teaching both at the undergraduate and postgraduate level with a special clinical interest in Women’s Health which has spanned comprehensive surgical obstetrical care across both high and low resource countries. Keyna has an academic fascination with the topic of optimal clinical learning environments and assessment in undergraduate medical education and is actively involved in several medical education research projects on that topic with both residents and undergraduate learners.
Apart from these scholarly interests and leadership roles, Dr. Bracken enjoys the promotion of Women’s Health care along with the concept of wellness and resilience both nationally and internationally and continues to work toward true reconciliation and the dismantling of the many systems of oppression and racism in both the learning and provision of health care both in Canada and internationally.
Special Interests: Optimal clinical learning environments, promotion of knowledge translation using learning psychology and technology assisted innovation, resilience and wellbeing over the course of medical education.
Keyna Bracken
BSc, MD, CCFP, FCFP
Professor
Chair Pre-Clerkship (UGME)
Keyna Bracken is a Professor in the Department of Family Medicine at McMaster University with a full time academic clinical practice at McMaster Family Practice. The former Undergraduate and Clerkship director for the department of Family Medicine, from 2016 until July 2022, Keyna is now the Chair Pre-Clerkship at the DeGroote School of Medicine where she actively works to champion the discipline of Family Medicine. Keyna is actively involved in teaching both at the undergraduate and postgraduate level with a special clinical interest in Women’s Health which has spanned comprehensive surgical obstetrical care across both high and low resource countries. Keyna has an academic fascination with the topic of optimal clinical learning environments and assessment in undergraduate medical education and is actively involved in several medical education research projects on that topic with both residents and undergraduate learners.
Apart from these scholarly interests and leadership roles, Dr. Bracken enjoys the promotion of Women’s Health care along with the concept of wellness and resilience both nationally and internationally and continues to work toward true reconciliation and the dismantling of the many systems of oppression and racism in both the learning and provision of health care both in Canada and internationally.
Special Interests: Optimal clinical learning environments, promotion of knowledge translation using learning psychology and technology assisted innovation, resilience and wellbeing over the course of medical education.
Martin Chasen
MBChB, FCP(SA), MPhil(Pall Med)
Clinical Professor
Dr. Chasen has been a faculty member of the Department of Family Medicine since 2016. He was born in Pretoria, South Africa, where completed his undergraduate training at the University of Pretoria in 1983, later obtaining a specialist degree in Internal Medicine, Medical Oncology, and Master of Philosophy (Palliative Medicine) at the University of Cape Town.
He is currently the Medical Director of Palliative Care at William Osler Health System in Brampton. He was previously the Medical Director of Palliative Care at The Ottawa Hospital Cancer Centre and the Palliative Rehabilitation Program at Élisabeth Bruyère Ottawa.
Dr. Chasen has over 110 peer-reviewed publications, abstracts, and book chapters. Presently, he is the principal investigator for the RELIEF App study, using digital technology to make palliative care accessible to people in their homes. Dr. Chasen is also involved in the development of European Society for Medical Oncology (ESMO) clinical practice guidelines for patients with anorexia-cachexia and the development of a Pan-Canadian guideline in survivorship. He has led 2 teams to achieve the international ESMO accreditation for Integrated Oncology/Palliative Centres.
Dr. Chasen has received multiple awards, including the Elizabeth J Latimer Prize in Palliative Care from McMaster University, Kay Blair Community Service Award from William Osler Health System, and Eduardo Bruera Award in Palliative Medicine from the CSPCP.
Outside of academia, Dr. Chasen enjoys spending time with his beautiful wife Pamela, two daughters, and two grandchildren. His enjoyment of arts and theatre is one of many of his passions.
Special Interests: Palliative care, survivorship, cancer cachexia, digital health technology.
Martin Chasen
MBChB, FCP(SA), MPhil(Pall Med)
Clinical Professor
Dr. Chasen has been a faculty member of the Department of Family Medicine since 2016. He was born in Pretoria, South Africa, where completed his undergraduate training at the University of Pretoria in 1983, later obtaining a specialist degree in Internal Medicine, Medical Oncology, and Master of Philosophy (Palliative Medicine) at the University of Cape Town.
He is currently the Medical Director of Palliative Care at William Osler Health System in Brampton. He was previously the Medical Director of Palliative Care at The Ottawa Hospital Cancer Centre and the Palliative Rehabilitation Program at Élisabeth Bruyère Ottawa.
Dr. Chasen has over 110 peer-reviewed publications, abstracts, and book chapters. Presently, he is the principal investigator for the RELIEF App study, using digital technology to make palliative care accessible to people in their homes. Dr. Chasen is also involved in the development of European Society for Medical Oncology (ESMO) clinical practice guidelines for patients with anorexia-cachexia and the development of a Pan-Canadian guideline in survivorship. He has led 2 teams to achieve the international ESMO accreditation for Integrated Oncology/Palliative Centres.
Dr. Chasen has received multiple awards, including the Elizabeth J Latimer Prize in Palliative Care from McMaster University, Kay Blair Community Service Award from William Osler Health System, and Eduardo Bruera Award in Palliative Medicine from the CSPCP.
Outside of academia, Dr. Chasen enjoys spending time with his beautiful wife Pamela, two daughters, and two grandchildren. His enjoyment of arts and theatre is one of many of his passions.
Special Interests: Palliative care, survivorship, cancer cachexia, digital health technology.
Amie Davis
MD, CCFP, FCFP
Associate Professor
Postgraduate Curriculum Director;
Medical Director, Maternity Centre of Hamilton
Dr. Amie Davis is a family physician in the Department of Family Medicine. For the first half of her career, she practiced community-based comprehensive family medicine which included adult inpatient, obstetrical, palliative and outpatient care. She was also the inaugural site director for the Halton Postgraduate Family Medicine residency site. Her work in medical education has allowed her to contribute in the roles of Site Director at many of the McMaster sites including Halton, Niagara and Hamilton. She is currently the Curriculum Director in the postgraduate Family Medicine program with a special interest in entrustment, competency-based learning and curriculum design. She became a full-time faculty member in 2019, and her family practice is located at Stonechurch Family Health centre where her special interests include delivering and teaching gender-affirming primary care, obstetrical care and women’s health. She is the current medical director of the Maternity Centre of Hamilton, where she participates in the collaborative model of expert family medicine obstetrical providers who provide antepartum, intrapartum and postpartum care to pregnant patients with a special expertise in providing care for pregnant people who may be socially at risk.
Special Interests: Family Medicine Obstetrical Care, Gender Affirming Primary Care, Medical Education.
Amie Davis
MD, CCFP, FCFP
Associate Professor
Postgraduate Curriculum Director;
Medical Director, Maternity Centre of Hamilton
Dr. Amie Davis is a family physician in the Department of Family Medicine. For the first half of her career, she practiced community-based comprehensive family medicine which included adult inpatient, obstetrical, palliative and outpatient care. She was also the inaugural site director for the Halton Postgraduate Family Medicine residency site. Her work in medical education has allowed her to contribute in the roles of Site Director at many of the McMaster sites including Halton, Niagara and Hamilton. She is currently the Curriculum Director in the postgraduate Family Medicine program with a special interest in entrustment, competency-based learning and curriculum design. She became a full-time faculty member in 2019, and her family practice is located at Stonechurch Family Health centre where her special interests include delivering and teaching gender-affirming primary care, obstetrical care and women’s health. She is the current medical director of the Maternity Centre of Hamilton, where she participates in the collaborative model of expert family medicine obstetrical providers who provide antepartum, intrapartum and postpartum care to pregnant patients with a special expertise in providing care for pregnant people who may be socially at risk.
Special Interests: Family Medicine Obstetrical Care, Gender Affirming Primary Care, Medical Education.
Erin Gallagher
BHSc, MD, CCFP (PC), MPH
Associate Professor
Dr. Erin Gallagher is a graduate of McMaster University’s Family Medicine residency program (2015), PGY3 Enhanced Skills Training in Palliative Care program (2016) and Master of Public Health program (2018). In 2017 she completed her Clinical Scholar training through McMaster Family Practice, followed by starting her own general practice in 2017 at Stonechurch Family Health Centre where she trained as a resident.
Through her undergraduate training, Dr. Gallagher discovered her love for medical education and leadership development of medical trainees, the latter being an area of research interest and publication. She is a clinical supervisor and lecturer at the undergraduate and postgraduate levels in the areas of general Family Medicine and Palliative Care. She sits on local, provincial and national committees for Palliative Care education for Family Medicine as well as Medicine and its Subspecialties. Her academic interests include public health approaches to palliative care, including community engagement and development, as well as building capacity for palliative care in primary care.
Clinically, Dr. Gallagher divides her time between providing comprehensive family medicine care to her patients and working as a palliative care consultant for McMaster’s Hamilton teaching sites and Hamilton Health Sciences hospitals. She is the Medical Director at Emmanuel House hospice in Hamilton and the Ontario Health West Physician Clinical Co-Lead for Palliative Care.
Erin Gallagher
BHSc, MD, CCFP (PC), MPH
Associate Professor
Dr. Erin Gallagher is a graduate of McMaster University’s Family Medicine residency program (2015), PGY3 Enhanced Skills Training in Palliative Care program (2016) and Master of Public Health program (2018). In 2017 she completed her Clinical Scholar training through McMaster Family Practice, followed by starting her own general practice in 2017 at Stonechurch Family Health Centre where she trained as a resident.
Through her undergraduate training, Dr. Gallagher discovered her love for medical education and leadership development of medical trainees, the latter being an area of research interest and publication. She is a clinical supervisor and lecturer at the undergraduate and postgraduate levels in the areas of general Family Medicine and Palliative Care. She sits on local, provincial and national committees for Palliative Care education for Family Medicine as well as Medicine and its Subspecialties. Her academic interests include public health approaches to palliative care, including community engagement and development, as well as building capacity for palliative care in primary care.
Clinically, Dr. Gallagher divides her time between providing comprehensive family medicine care to her patients and working as a palliative care consultant for McMaster’s Hamilton teaching sites and Hamilton Health Sciences hospitals. She is the Medical Director at Emmanuel House hospice in Hamilton and the Ontario Health West Physician Clinical Co-Lead for Palliative Care.
Lawrence Grierson
PhD
Associate Professor
Assistant Dean, Health Sciences Education Graduate Program (HSED); Scientist, McMaster Education Research, Innovation, and Theory (MERIT)
Dr. Lawrence Grierson leads research concerned with understanding the relationship between health professions education policies and practices and the quality of healthcare delivered to patients and communities. This work pays specific attention to education antecedents for effective comprehensive family medicine practice, training approaches that promote the acquisition of clinical technical skills, and the ethical inter-institutional collation of training metrics for medical education research.
Dr. Grierson is a member of the Canadian Association of Medical Educators and the CFPC Section of Researchers. He is Associate Professor with the Department of Family Medicine (DFM); Assistant Dean of the Health Sciences Education Graduate Program (HSED); and Scientist with the McMaster FHS Program for Education Research, Innovation, & Theory (MERIT).
Special Interests: Medical and health professions education, admissions and assessment, education research data management, precision technical skills.
Lawrence Grierson
PhD
Associate Professor
Assistant Dean, Health Sciences Education Graduate Program (HSED); Scientist, McMaster Education Research, Innovation, and Theory (MERIT)
Dr. Lawrence Grierson leads research concerned with understanding the relationship between health professions education policies and practices and the quality of healthcare delivered to patients and communities. This work pays specific attention to education antecedents for effective comprehensive family medicine practice, training approaches that promote the acquisition of clinical technical skills, and the ethical inter-institutional collation of training metrics for medical education research.
Dr. Grierson is a member of the Canadian Association of Medical Educators and the CFPC Section of Researchers. He is Associate Professor with the Department of Family Medicine (DFM); Assistant Dean of the Health Sciences Education Graduate Program (HSED); and Scientist with the McMaster FHS Program for Education Research, Innovation, & Theory (MERIT).
Special Interests: Medical and health professions education, admissions and assessment, education research data management, precision technical skills.
Dale Guenter
MD, MPH
Professor Emeritus
Faculty Experience Director
Dale Guenter has experience in community-oriented primary care among populations living on the margins of society and the health system, including people in the inner city, remote northern communities, the Philippines, and people experiencing incarceration. He has been focused clinically on managing illness from blood-born pathogens, chronic pain, addiction and mental health issues. He has pursued teaching, research and program development relevant to all of these areas. The emphasis in all of his work is to learn new ways to be profoundly relationship-centred, equity-seeking, and system-improving. His clinical role is with Shelter Health Network in Hamilton. He works to humanize the experience family medicine faculty members in his role as the Faculty Experience Director.
Dale Guenter
MD, MPH
Professor Emeritus
Faculty Experience Director
Dale Guenter has experience in community-oriented primary care among populations living on the margins of society and the health system, including people in the inner city, remote northern communities, the Philippines, and people experiencing incarceration. He has been focused clinically on managing illness from blood-born pathogens, chronic pain, addiction and mental health issues. He has pursued teaching, research and program development relevant to all of these areas. The emphasis in all of his work is to learn new ways to be profoundly relationship-centred, equity-seeking, and system-improving. His clinical role is with Shelter Health Network in Hamilton. He works to humanize the experience family medicine faculty members in his role as the Faculty Experience Director.
Michelle Howard
BA (Hons), MSc, PhD
Associate Professor
Michelle Howard is an Associate Professor in the Department of Family Medicine. Her research focuses on understanding the role of primary care for people with serious and life-limiting illness, by examining the influences of practice models, patterns and policies using health administrative and clinical data. She has also studied how patients and health care professionals in primary care talk about serious illness and preparing for future decision-making and has evaluated several tools for advance care planning in family practice.
Michelle has an MSc in Epidemiology from the University of Toronto and a PhD in Health Research Methodology from McMaster University. She primarily uses quantitative approaches including observational studies with population-based data (e.g. www.ices.on.ca www.cpcssn.ca), survey research and development of measures.
Michelle is an instructor for the Program Evaluation course in the McMaster Health Science Education (HSED) program and supervises graduate students with relevant research interests in McMaster’s Health Research Methodology Program.
Michelle Howard
BA (Hons), MSc, PhD
Associate Professor
Michelle Howard is an Associate Professor in the Department of Family Medicine. Her research focuses on understanding the role of primary care for people with serious and life-limiting illness, by examining the influences of practice models, patterns and policies using health administrative and clinical data. She has also studied how patients and health care professionals in primary care talk about serious illness and preparing for future decision-making and has evaluated several tools for advance care planning in family practice.
Michelle has an MSc in Epidemiology from the University of Toronto and a PhD in Health Research Methodology from McMaster University. She primarily uses quantitative approaches including observational studies with population-based data (e.g. www.ices.on.ca www.cpcssn.ca), survey research and development of measures.
Michelle is an instructor for the Program Evaluation course in the McMaster Health Science Education (HSED) program and supervises graduate students with relevant research interests in McMaster’s Health Research Methodology Program.
Gabrielle Inglis
MD, MMSc, CCFP
Assistant Professor (on leave)
Gabrielle Inglis joined the Department of Family Medicine as an Assistant Professor in 2019. In addition to her clinical practice at McMaster Family Practice, she works as a Consultant Physician with the Inpatient Addiction Medicine Service at Hamilton Health Sciences and St. Joseph’s Hospital. Prior to joining the department, she completed a Masters in Medical Education at Harvard University, and is actively involved in post-graduate and undergraduate medical education.
Special Interests: Care for People who use Drugs, Primary care generalism, Medical Education, Narrative Medicine
Gabrielle Inglis
MD, MMSc, CCFP
Assistant Professor (on leave)
Gabrielle Inglis joined the Department of Family Medicine as an Assistant Professor in 2019. In addition to her clinical practice at McMaster Family Practice, she works as a Consultant Physician with the Inpatient Addiction Medicine Service at Hamilton Health Sciences and St. Joseph’s Hospital. Prior to joining the department, she completed a Masters in Medical Education at Harvard University, and is actively involved in post-graduate and undergraduate medical education.
Special Interests: Care for People who use Drugs, Primary care generalism, Medical Education, Narrative Medicine
Fiona Kouyoumdjian
MD, MPH, PhD, FCFP, FRCPC
Research Director & Assistant Professor
Fiona Kouyoumdjian is a Family Physician, Public Health and Preventive Medicine Physician, and Epidemiologist. She received her BA with Honors from Brown University, her MD from Dalhousie University, her MPH from the Johns Hopkins Bloomberg School of Public Health, and her PhD in Epidemiology from the University of Toronto Dalla Lana School of Public Health. She completed residency training at the University of Toronto and a CIHR Fellowship at St. Michael’s Hospital.
Fiona leads a program of research focused on the health status and health care of people who experience imprisonment. Her specific research foci are decreasing imprisonment, improving health care and health promotion for people in prison, and supporting successful re-integration to the community for people on release from prison.
Fiona is also an Adjunct Scientist at ICES and an Associate Member in the Department of Health Research Methods, Evidence, and Impact at McMaster.
Fiona Kouyoumdjian
MD, MPH, PhD, FCFP, FRCPC
Research Director & Assistant Professor
Fiona Kouyoumdjian is a Family Physician, Public Health and Preventive Medicine Physician, and Epidemiologist. She received her BA with Honors from Brown University, her MD from Dalhousie University, her MPH from the Johns Hopkins Bloomberg School of Public Health, and her PhD in Epidemiology from the University of Toronto Dalla Lana School of Public Health. She completed residency training at the University of Toronto and a CIHR Fellowship at St. Michael’s Hospital.
Fiona leads a program of research focused on the health status and health care of people who experience imprisonment. Her specific research foci are decreasing imprisonment, improving health care and health promotion for people in prison, and supporting successful re-integration to the community for people on release from prison.
Fiona is also an Adjunct Scientist at ICES and an Associate Member in the Department of Health Research Methods, Evidence, and Impact at McMaster.
Linda Lee
MD, CCFP(COE), FCFP, MClSc
Associate Clinical Professor
Dr. Linda Lee is a Care of the Elderly family physician, Associate Clinical Professor in the Department of Family Medicine at McMaster University, Director of the Centre for Family Medicine and KW Regional Memory Clinics, and Schlegel Chair in Primary Care for Elders. She has developed the MINT Memory Clinic model and Training Program which has assisted 120 other primary care settings in Ontario, BC, Alberta, and Saskatchewan to establish new MINT Memory Clinics. Dr. Lee’s research interests focus on improving health care for older adults living with dementia and other complex chronic conditions. She enjoys time with family, growing tomatoes, and raising parrots.
Special Interests: community-based dementia care, frailty in primary care.
Linda Lee
MD, CCFP(COE), FCFP, MClSc
Associate Clinical Professor
Dr. Linda Lee is a Care of the Elderly family physician, Associate Clinical Professor in the Department of Family Medicine at McMaster University, Director of the Centre for Family Medicine and KW Regional Memory Clinics, and Schlegel Chair in Primary Care for Elders. She has developed the MINT Memory Clinic model and Training Program which has assisted 120 other primary care settings in Ontario, BC, Alberta, and Saskatchewan to establish new MINT Memory Clinics. Dr. Lee’s research interests focus on improving health care for older adults living with dementia and other complex chronic conditions. She enjoys time with family, growing tomatoes, and raising parrots.
Special Interests: community-based dementia care, frailty in primary care.
Robin Lennox
MD, CCFP
Assistant Clinical Professor
Robin Lennox has been a Family Physician and Assistant Professor with the Department of Family Medicine since 2017. She has a clinical focus in the care of people who use drugs, which includes working with the Rapid Access Addiction Medicine Clinic and the Program for Substance Use in Pregnancy at the Maternity Centre of Hamilton. She is co-Head of Service for the Inpatient Addiction Medicine Service at Hamilton Health Sciences and St. Joseph’s Healthcare Hamilton. In addition, Dr. Lennox works with the Shelter Health Network providing primary care for people deprived of housing. She has a diverse research portfolio aimed at improving models of care delivery and the health outcomes of people who use drugs with infectious complications, and improving the experiences of people who use drugs when interacting with the health system.
Special Interests: Care of People Who Use Drugs, Addiction Medicine, HIV primary care, gender diverse care, care of people deprived of housing.
Robin Lennox
MD, CCFP
Assistant Clinical Professor
Robin Lennox has been a Family Physician and Assistant Professor with the Department of Family Medicine since 2017. She has a clinical focus in the care of people who use drugs, which includes working with the Rapid Access Addiction Medicine Clinic and the Program for Substance Use in Pregnancy at the Maternity Centre of Hamilton. She is co-Head of Service for the Inpatient Addiction Medicine Service at Hamilton Health Sciences and St. Joseph’s Healthcare Hamilton. In addition, Dr. Lennox works with the Shelter Health Network providing primary care for people deprived of housing. She has a diverse research portfolio aimed at improving models of care delivery and the health outcomes of people who use drugs with infectious complications, and improving the experiences of people who use drugs when interacting with the health system.
Special Interests: Care of People Who Use Drugs, Addiction Medicine, HIV primary care, gender diverse care, care of people deprived of housing.
Dee Mangin
MBChB, FRNZCGP, DPH
Professor (Part-Time)
Derelie (Dee) Mangin is a professor in the Department of Family Medicine, where she has held the distinguished David Braley Nancy Gordon Chair since 2013. Her academic interests include the role and value of generalist primary care; innovative models of primary care delivery; rational prescribing; effective incorporation of evidence into patient centered practice; and the influences of science, policy and commerce on the nature of care. An area of current focus is multimorbidity and polypharmacy among older adults as a lens for promoting care that maps onto patient priorities and where the burden or care does not exceed the patient’s capacity to benefit. She has wide clinical research experience in primary care, including observational and interventional quantitative research methods and community randomized control trials (RCTs) of innovative models of care. She is currently director of the McMaster University Sentinel and Information Collaboration (MUSIC) practice based research network. Dee has experience leading RCTs of clinical interventions in areas such as antidepressant use, community acquired pneumonia, antibiotics in urinary tract infections, and deprescription trials. She has received award for leadership in Family Medicine and in Family Medicine research that include the Royal New Zealand College of General Practitioners Distinguished Service Award and the Canadian College of Family Physicians Donald I Rice Award.
Special Interests: The role and value of generalist primary care in the health system; innovative models of primary care delivery; rational prescribing; effective incorporation of evidence into patient centered practice; and the influences of science, policy and commerce on the nature of care.
Dee Mangin
MBChB, FRNZCGP, DPH
Professor (Part-Time)
Derelie (Dee) Mangin is a professor in the Department of Family Medicine, where she has held the distinguished David Braley Nancy Gordon Chair since 2013. Her academic interests include the role and value of generalist primary care; innovative models of primary care delivery; rational prescribing; effective incorporation of evidence into patient centered practice; and the influences of science, policy and commerce on the nature of care. An area of current focus is multimorbidity and polypharmacy among older adults as a lens for promoting care that maps onto patient priorities and where the burden or care does not exceed the patient’s capacity to benefit. She has wide clinical research experience in primary care, including observational and interventional quantitative research methods and community randomized control trials (RCTs) of innovative models of care. She is currently director of the McMaster University Sentinel and Information Collaboration (MUSIC) practice based research network. Dee has experience leading RCTs of clinical interventions in areas such as antidepressant use, community acquired pneumonia, antibiotics in urinary tract infections, and deprescription trials. She has received award for leadership in Family Medicine and in Family Medicine research that include the Royal New Zealand College of General Practitioners Distinguished Service Award and the Canadian College of Family Physicians Donald I Rice Award.
Special Interests: The role and value of generalist primary care in the health system; innovative models of primary care delivery; rational prescribing; effective incorporation of evidence into patient centered practice; and the influences of science, policy and commerce on the nature of care.
Anjali Menezes
Assistant Clinical Professor (Adjunct)
Anjali Menezes
Assistant Clinical Professor (Adjunct)
James Milligan
BSc.P.T., MD, CCFP, FCFP
Assistant Clinical Professor
Family physician with the Centre for Family Medicine (CFFM) Kitchener-Waterloo. Director of the CFFM Mobility Clinic, an interprofessional primary care clinic with a focus to improve primary care for individuals with spinal cord injury and other physical disabilities. The clinic is dedicated to clinical research in primary care, working closely with the Praxis Spinal Cord Injury Institute. Associate Clinical Professor with the McMaster University Department of Family Medicine and Clinical Specialist for Mobility and Falls with the University of Waterloo-Schlegel Research Institute for Aging (UW-RIA).
Special Interests: Director Mobility Clinic. Interest in primary care research involving spinal cord injury and physical disabilities.
James Milligan
BSc.P.T., MD, CCFP, FCFP
Assistant Clinical Professor
Family physician with the Centre for Family Medicine (CFFM) Kitchener-Waterloo. Director of the CFFM Mobility Clinic, an interprofessional primary care clinic with a focus to improve primary care for individuals with spinal cord injury and other physical disabilities. The clinic is dedicated to clinical research in primary care, working closely with the Praxis Spinal Cord Injury Institute. Associate Clinical Professor with the McMaster University Department of Family Medicine and Clinical Specialist for Mobility and Falls with the University of Waterloo-Schlegel Research Institute for Aging (UW-RIA).
Special Interests: Director Mobility Clinic. Interest in primary care research involving spinal cord injury and physical disabilities.
Margo Mountjoy
MD, PhD, CCFP(SEM), FCFP, FACSM, Dip Sport Med.
Clinical Professor
Dr. Mountjoy is a Clinical Professor in the Department of Family Medicine at McMaster University Medical School and Regional Assistant Dean of the Michael G. DeGroote School of Medicine, McMaster University. She is also a clinician scientist – working for several International Sports organizations in the field of sports medicine including the International Olympic Committee (Games Group), the Association of Summer Olympic International Federations, FIFA, International Golf Federation, World Rugby, and for the World Anti-Doping Agency. She is a retired elite synchronized swimmer. One of her areas of expertise is in the field of harassment + abuse in sport, athlete mental health and female athlete health She is an active advocate of athlete health and well-being at the national and international levels.
Special Interests: Sport and exercise medicine, medical education.
Margo Mountjoy
MD, PhD, CCFP(SEM), FCFP, FACSM, Dip Sport Med.
Clinical Professor
Dr. Mountjoy is a Clinical Professor in the Department of Family Medicine at McMaster University Medical School and Regional Assistant Dean of the Michael G. DeGroote School of Medicine, McMaster University. She is also a clinician scientist – working for several International Sports organizations in the field of sports medicine including the International Olympic Committee (Games Group), the Association of Summer Olympic International Federations, FIFA, International Golf Federation, World Rugby, and for the World Anti-Doping Agency. She is a retired elite synchronized swimmer. One of her areas of expertise is in the field of harassment + abuse in sport, athlete mental health and female athlete health She is an active advocate of athlete health and well-being at the national and international levels.
Special Interests: Sport and exercise medicine, medical education.
Danielle O'Toole
MD, CCFP
Associate Professor
Danielle O'Toole
MD, CCFP
Associate Professor
Doug Oliver
BSc, MSc, MD, CCFP
Associate Professor
Medical Director, McMaster Family Practice
Dr. Oliver is an Associate Professor in the Department of Family Medicine at McMaster University.
He joined the Department in 2004 and took on a full-time faculty position in 2007.
Dr. Oliver’s passion for elder care lead him to take on the position as Care of the Elderly Curriculum Coordinator from 2006 – 2015. This role allowed him to develop many innovative programs for the Department, including a Long Term Care clinical rotation for residents and a successful annual CME event entitled “Care of the Elderly: Perspectives for Primary Care”. His clinical commitment to this patient population continues with weekly nursing home rounds and house-calls to frail elderly patients.
He is also co-PI on Health Tapestry, a multi-year, multi-site primary care based intervention aimed at promoting optimal aging in community dwelling older adults. Dr. Oliver’s interest in improving access for patients in primary care resulted in study and co-development of an Advanced Access booking model in the McMaster Family Health Team. This model allows patients better access to their primary care team by having the majority of booking spots available for same day appointments.
Dr. Oliver is the Principle Investigator on a research project designed to better understand how and why patients make the choices they do, when calling in to book an appointment with their family doctor. On the academic front, Dr. Oliver is assisting the Department with several educational leadership roles including Co-Education Coordinator at McMaster Family Practice (2011-16), Hamilton Site Director and CBRT Education Coordinator (2012-2013) and Behavioural Sciences Co-Coordinator (2013-).
Dr. Oliver has held several academic leadership roles in the last few years, including Education Coordinator at MFP (2011-16), MHBS Curriculum Coordinator (2013-2019) and is currently the Medical Director at McMaster Family Practice (2016-present)”
Doug Oliver
BSc, MSc, MD, CCFP
Associate Professor
Medical Director, McMaster Family Practice
Dr. Oliver is an Associate Professor in the Department of Family Medicine at McMaster University.
He joined the Department in 2004 and took on a full-time faculty position in 2007.
Dr. Oliver’s passion for elder care lead him to take on the position as Care of the Elderly Curriculum Coordinator from 2006 – 2015. This role allowed him to develop many innovative programs for the Department, including a Long Term Care clinical rotation for residents and a successful annual CME event entitled “Care of the Elderly: Perspectives for Primary Care”. His clinical commitment to this patient population continues with weekly nursing home rounds and house-calls to frail elderly patients.
He is also co-PI on Health Tapestry, a multi-year, multi-site primary care based intervention aimed at promoting optimal aging in community dwelling older adults. Dr. Oliver’s interest in improving access for patients in primary care resulted in study and co-development of an Advanced Access booking model in the McMaster Family Health Team. This model allows patients better access to their primary care team by having the majority of booking spots available for same day appointments.
Dr. Oliver is the Principle Investigator on a research project designed to better understand how and why patients make the choices they do, when calling in to book an appointment with their family doctor. On the academic front, Dr. Oliver is assisting the Department with several educational leadership roles including Co-Education Coordinator at McMaster Family Practice (2011-16), Hamilton Site Director and CBRT Education Coordinator (2012-2013) and Behavioural Sciences Co-Coordinator (2013-).
Dr. Oliver has held several academic leadership roles in the last few years, including Education Coordinator at MFP (2011-16), MHBS Curriculum Coordinator (2013-2019) and is currently the Medical Director at McMaster Family Practice (2016-present)”
David Price
BSc, MD, CCFP, FCFP
Professor
Dr. David Price – Professor and Past-Chair (2006-2021), Department of Family Medicine at McMaster University. During his tenure as chair, the Department grew exponentially, graduating over 100 family medicine residents annually in what is generally acknowledged to be one of the top academic programs in the country. As part of the residency expansion; teaching units and/or Family Health Teams (FHT) were created in a number of communities in south central Ontario. Department owned and managed teaching sites include Burlington, Stonechurch and MFP. He was the founding director of the Maternity Centre of Hamilton; a multidisciplinary centre that cares for prenatal and intrapartum patients. Dr. Price was also instrumental in helping to create the academic FHT at McMaster University, an interprofessional team, currently serving over 40,000 patients in the Hamilton area. He was a key player in the development of the $85 M, David Braley Health Sciences Centre, a six-story, 185,000 sq. ft. home for Family Medicine and Hamilton Public Health in the downtown core. The research enterprise of the department has also grown in size and reputation, managing over $10M in research grants annually. He also led the creation of a second endowed chair in family medicine ($2 million), the Niagara professorship ($1 million) and the establishment of the David Braley Primary Care Research Collaborative with an additional $4 million endowment.
Through his leadership roles at the University and Hospital (Chief of Family Medicine at Hamilton Health Sciences from 2004-2018), and his involvement with local, regional, and provincial government bodies where he acts as a consultant and advisor, he has developed expertise in primary care reform and health care policy development. He has provided his expertise to provincial governments in Canada, as well as internationally. He has enjoyed learning about other primary care systems around the world during his many visits as an invited speaker to numerous countries.
As the Chair of the Provincial (Ontario) Expert Advisory Panel on Primary Care (2013-2014) he was instrumental in helping produce “Patient Care Groups: A new model of population based primary health care for Ontario” (“Price Report”). He is currently the chair of the Minister of Health’s Primary Care Advisory Table, and has been on Ontario’s Covid-19 Health Coordination Table since April 2020. At the University, he is chair of the Faculty of Health Sciences Finance Committee, and as Secretary of Regional Medical Associates, the incoming president (fall 2022). In July 2021, he became the co-lead of the Health Leadership Academy (a partnership between the DeGroote School of Medicine and DeGroote School of Business).
David Price
BSc, MD, CCFP, FCFP
Professor
Dr. David Price – Professor and Past-Chair (2006-2021), Department of Family Medicine at McMaster University. During his tenure as chair, the Department grew exponentially, graduating over 100 family medicine residents annually in what is generally acknowledged to be one of the top academic programs in the country. As part of the residency expansion; teaching units and/or Family Health Teams (FHT) were created in a number of communities in south central Ontario. Department owned and managed teaching sites include Burlington, Stonechurch and MFP. He was the founding director of the Maternity Centre of Hamilton; a multidisciplinary centre that cares for prenatal and intrapartum patients. Dr. Price was also instrumental in helping to create the academic FHT at McMaster University, an interprofessional team, currently serving over 40,000 patients in the Hamilton area. He was a key player in the development of the $85 M, David Braley Health Sciences Centre, a six-story, 185,000 sq. ft. home for Family Medicine and Hamilton Public Health in the downtown core. The research enterprise of the department has also grown in size and reputation, managing over $10M in research grants annually. He also led the creation of a second endowed chair in family medicine ($2 million), the Niagara professorship ($1 million) and the establishment of the David Braley Primary Care Research Collaborative with an additional $4 million endowment.
Through his leadership roles at the University and Hospital (Chief of Family Medicine at Hamilton Health Sciences from 2004-2018), and his involvement with local, regional, and provincial government bodies where he acts as a consultant and advisor, he has developed expertise in primary care reform and health care policy development. He has provided his expertise to provincial governments in Canada, as well as internationally. He has enjoyed learning about other primary care systems around the world during his many visits as an invited speaker to numerous countries.
As the Chair of the Provincial (Ontario) Expert Advisory Panel on Primary Care (2013-2014) he was instrumental in helping produce “Patient Care Groups: A new model of population based primary health care for Ontario” (“Price Report”). He is currently the chair of the Minister of Health’s Primary Care Advisory Table, and has been on Ontario’s Covid-19 Health Coordination Table since April 2020. At the University, he is chair of the Faculty of Health Sciences Finance Committee, and as Secretary of Regional Medical Associates, the incoming president (fall 2022). In July 2021, he became the co-lead of the Health Leadership Academy (a partnership between the DeGroote School of Medicine and DeGroote School of Business).
Amanda Ramdyal
MD, CCFP, MSc
Assistant Professor
Education Coordinator
Dr. Amanda Ramdyal is Family Physician and joined the Department of Family Medicine in 2016 as a locum, and then became an Assistant Professor in 2017. She has a strong clinical interest in women’s health and sexual health. Dr. Ramdyal is a staff physician at Stonechurch Family Health Centre, as well as with Hamilton Public Health Sexual Health Clinic. She has a special research interest in prevention, screening and management of sexually transmitted infections.
Amanda Ramdyal
MD, CCFP, MSc
Assistant Professor
Education Coordinator
Dr. Amanda Ramdyal is Family Physician and joined the Department of Family Medicine in 2016 as a locum, and then became an Assistant Professor in 2017. She has a strong clinical interest in women’s health and sexual health. Dr. Ramdyal is a staff physician at Stonechurch Family Health Centre, as well as with Hamilton Public Health Sexual Health Clinic. She has a special research interest in prevention, screening and management of sexually transmitted infections.
Lynda Redwood-Campbell
MD, FCFP, MPH
Professor
Dr. Redwood-Campbell is a full-time faculty member and Full Professor in the Department of Family Medicine since 1996. She is the co-director, Global Health for Postgraduate Medical Education McMaster University. She has a keen interest and expertise in Global Health. She completed her MD and residency at McMaster and her Diploma in Hygiene and Public Health in London UK at the London School of Tropical Medicine and Hygiene. She additionally completed her Master’s in Public Health at Johns Hopkins Bloomberg School of Public Health. She has been involved in global health partnerships in primary care and global family medicine. She is the current Chair, Besrour Global Family Medicine Advisory Council. She has decades of experience international disaster humanitarian work mostly with the Canadian and International Red Cross. She has worked in many countries like Indonesia, Bangladesh, the Philippines, Haiti, Mozambique, Nepal and more. She is the recipient of the OMA Presidential Award, which recognizes long-standing humanitarian service to the greater community. Her more recent research focused on lessons learned by healthcare teams doing international humanitarian work and how this is directly applicable to the Canadian context. In 2023, she is a member of the Ontario Public Health Emergencies Science Advisory Council. She enjoys teaching medical residents and students in a broad family medicine context. Dr. Redwood-Campbell has a clinical practice at McMaster University and enjoys the Canadian outdoors. Further information can be found at https://mcmasterfamilypractice.ca/bios/lynda-redwood-campbell/
Special Interests: Global Health, humanitarian response, complex humanitarian emergencies, immigrant and refugee health, primary health care, global family medicine, equity in healthcare, medical education, teaching in medicine, quality assurance.
Lynda Redwood-Campbell
MD, FCFP, MPH
Professor
Dr. Redwood-Campbell is a full-time faculty member and Full Professor in the Department of Family Medicine since 1996. She is the co-director, Global Health for Postgraduate Medical Education McMaster University. She has a keen interest and expertise in Global Health. She completed her MD and residency at McMaster and her Diploma in Hygiene and Public Health in London UK at the London School of Tropical Medicine and Hygiene. She additionally completed her Master’s in Public Health at Johns Hopkins Bloomberg School of Public Health. She has been involved in global health partnerships in primary care and global family medicine. She is the current Chair, Besrour Global Family Medicine Advisory Council. She has decades of experience international disaster humanitarian work mostly with the Canadian and International Red Cross. She has worked in many countries like Indonesia, Bangladesh, the Philippines, Haiti, Mozambique, Nepal and more. She is the recipient of the OMA Presidential Award, which recognizes long-standing humanitarian service to the greater community. Her more recent research focused on lessons learned by healthcare teams doing international humanitarian work and how this is directly applicable to the Canadian context. In 2023, she is a member of the Ontario Public Health Emergencies Science Advisory Council. She enjoys teaching medical residents and students in a broad family medicine context. Dr. Redwood-Campbell has a clinical practice at McMaster University and enjoys the Canadian outdoors. Further information can be found at https://mcmasterfamilypractice.ca/bios/lynda-redwood-campbell/
Special Interests: Global Health, humanitarian response, complex humanitarian emergencies, immigrant and refugee health, primary health care, global family medicine, equity in healthcare, medical education, teaching in medicine, quality assurance.
Cathy Risdon
MD, DMan, CCFP, FCFP
Professor & Chair
Dr. Cathy Risdon is Professor and Chair of the Department of Family Medicine at McMaster aiming to help reinvigorate a sustainable, inclusive learning and practice environment for current and future family medicine learners and providers. For Risdon, breaking down barriers and honouring different viewpoints is key to building a successful department capable of training top-quality family doctors and attracting skilled staff and faculty.
She was the first holder of the David Braley-Nancy Gordon Endowed Chair in Family Medicine, mandated to develop innovations in education, clinical service and research relating to the doctor-patient and interdisciplinary team relationships. She co-created the Michael G. DeGroote School of Medicine’s Professional Competency Curriculum, a two-year course to teach professionalism, communication skills, advocacy, ethics and reflective practice. Following the ten-year term of her Endowed Chair, she became Associate Chair, Academic within the Department of Family Medicine, as well as the co-lead for the McMaster Family Health Team.
Dr. Risdon has completed a Doctorate of Management in Organizational Change at the University of Hertfordshire where her research explored themes of excellence and improvisation within curriculum design and implementation. She has conducted training and consultations across North America for primary care and community-based agencies wishing to improve their capacity for effective team and interprofessional collaborations. Her expertise in facilitation was used to design and deliver on the successful Hamilton Health Team submission. She is an expert in health system integration and primary care and is one of three Canadians who has been inducted as a Fellow of the Academy of Communications in Healthcare in recognition of her contributions to curricular design and facilitation.
A McMaster graduate (class of ’92), Dr. Risdon’s clinical practice has included a varied inner-city population with a focus on vulnerable populations.
After more than 30 years in the Department of Family Medicine at McMaster, Dr. Risdon is still amazed at her good fortune in working with such terrific people. “We have extraordinary people engaged in our mission of service, teaching, and discovery. It’s my privilege to do all that I can to help them thrive.”
Cathy Risdon
MD, DMan, CCFP, FCFP
Professor & Chair
Dr. Cathy Risdon is Professor and Chair of the Department of Family Medicine at McMaster aiming to help reinvigorate a sustainable, inclusive learning and practice environment for current and future family medicine learners and providers. For Risdon, breaking down barriers and honouring different viewpoints is key to building a successful department capable of training top-quality family doctors and attracting skilled staff and faculty.
She was the first holder of the David Braley-Nancy Gordon Endowed Chair in Family Medicine, mandated to develop innovations in education, clinical service and research relating to the doctor-patient and interdisciplinary team relationships. She co-created the Michael G. DeGroote School of Medicine’s Professional Competency Curriculum, a two-year course to teach professionalism, communication skills, advocacy, ethics and reflective practice. Following the ten-year term of her Endowed Chair, she became Associate Chair, Academic within the Department of Family Medicine, as well as the co-lead for the McMaster Family Health Team.
Dr. Risdon has completed a Doctorate of Management in Organizational Change at the University of Hertfordshire where her research explored themes of excellence and improvisation within curriculum design and implementation. She has conducted training and consultations across North America for primary care and community-based agencies wishing to improve their capacity for effective team and interprofessional collaborations. Her expertise in facilitation was used to design and deliver on the successful Hamilton Health Team submission. She is an expert in health system integration and primary care and is one of three Canadians who has been inducted as a Fellow of the Academy of Communications in Healthcare in recognition of her contributions to curricular design and facilitation.
A McMaster graduate (class of ’92), Dr. Risdon’s clinical practice has included a varied inner-city population with a focus on vulnerable populations.
After more than 30 years in the Department of Family Medicine at McMaster, Dr. Risdon is still amazed at her good fortune in working with such terrific people. “We have extraordinary people engaged in our mission of service, teaching, and discovery. It’s my privilege to do all that I can to help them thrive.”
Inge Schabort
MBChB, BScMedScHons (Epi), BScMedScHons (Med Biochem), MSc(EBHC), MHPE, CCFP, FCFP
Associate Professor, Full-time Academic Family Physician, Postgraduate IMG Director
Dr. Inge Schabort is an Associate Professor of Family Medicine and the Postgraduate International Medical Graduate (IMG) Director at the Department of Family Medicine, McMaster University. She practices as a full-time academic family physician at Stonechurch Family Health Centre and she tutors Evidence-Based Medicine, Quality Improvement and Mental Health and Behavioural Sciences in the residency program She just completed her term as Academic Half Day Coordinator in the Department.
Dr Schabort recently completed a Master of Health Professions Education (MHPE) at the University of Maastricht in the Netherlands (2020) and an MSc in Evidence Based Health Care from Oxford University in the UK (2022).
After medical school she worked as a physician in Sub-Saharan Africa for 10 years and completed postgraduate training in obstetrics and gynecology, internal medicine, epidemiology, immunology, endocrinology, biochemistry and pathology before she was recruited to Canada. In Canada it took several years for her to compete for an IMG position in Ontario and then repeat her clerkship as well as complete a family medicine residency in the Ontario IMG program.
Dr. Schabort is an author of the national Future of Medical Education in Canada (FMEC) IMG Environmental Scan document, and she also was a physician-stakeholder consultant for the Pan-Canadian Framework for the Assessment and recognition of foreign qualifications for the entry to Residency pathway. She sat on the Thomson IMG Working Group of the Council of Ontario Universities and is currently representing the CFPC on the national N4 Working Group to leverage IMGs to close healthcare labour market gaps. She completed a comprehensive review of the medical student and resident selection and IMG literature and has published research on IMG selection predictors for success. Her MHPE thesis studied IMG selection in Canada and her Oxford dissertation studied IMGs internationally. She recently completed a systematic review of prognostic studies on predictors for success in IMGs in postgraduate training and practice internationally as part of her Oxford dissertation. She currently sits on the Board of Directors of the Canadian Residency Matching Service as an expert in IMG matters.
Dr. Schabort was on the Ontario Steering Committee for the development of the Curriculum for the Ontario International Medical Graduate Pre-Residency program and currently is on the Curricular Advisory Committee for the Pre-residency IMG program for all RCPSC and CFPC IMGs entering residency training in Ontario. She sat on the provincial steering committee for the development of the curriculum and selection process for Practice Ready Assessment. She sat on the Steering Committee for the Ontario Inter-professional Spinal Assessment Education Clinics (ISAEC) and was the Hamilton Primary Care Lead for the implementation of the ISAEC pilot.
She has authored papers on several topics in medical education and primary care research, and an invited book chapter on International Medical Graduates. She has received several awards including the 2012 Award of Excellence from the College of Family Physicians of Canada and the Glenn Sawyer Service Award from the Ontario Medical Association in 2015 as well as the Professional Association of Residents of Ontario (PARO) Excellence in Clinical Teaching Award in 2021
Her clinical and academic interests include medical education, selection, assessment, remediation, leadership, mentorship, IMG education and advocacy, disease screening, prevention and health promotion global health, inter-professional care and education, vulnerable population health, women’s health, chronic disease management, evidence-based medicine and primary care research.
Inge Schabort
MBChB, BScMedScHons (Epi), BScMedScHons (Med Biochem), MSc(EBHC), MHPE, CCFP, FCFP
Associate Professor, Full-time Academic Family Physician, Postgraduate IMG Director
Dr. Inge Schabort is an Associate Professor of Family Medicine and the Postgraduate International Medical Graduate (IMG) Director at the Department of Family Medicine, McMaster University. She practices as a full-time academic family physician at Stonechurch Family Health Centre and she tutors Evidence-Based Medicine, Quality Improvement and Mental Health and Behavioural Sciences in the residency program She just completed her term as Academic Half Day Coordinator in the Department.
Dr Schabort recently completed a Master of Health Professions Education (MHPE) at the University of Maastricht in the Netherlands (2020) and an MSc in Evidence Based Health Care from Oxford University in the UK (2022).
After medical school she worked as a physician in Sub-Saharan Africa for 10 years and completed postgraduate training in obstetrics and gynecology, internal medicine, epidemiology, immunology, endocrinology, biochemistry and pathology before she was recruited to Canada. In Canada it took several years for her to compete for an IMG position in Ontario and then repeat her clerkship as well as complete a family medicine residency in the Ontario IMG program.
Dr. Schabort is an author of the national Future of Medical Education in Canada (FMEC) IMG Environmental Scan document, and she also was a physician-stakeholder consultant for the Pan-Canadian Framework for the Assessment and recognition of foreign qualifications for the entry to Residency pathway. She sat on the Thomson IMG Working Group of the Council of Ontario Universities and is currently representing the CFPC on the national N4 Working Group to leverage IMGs to close healthcare labour market gaps. She completed a comprehensive review of the medical student and resident selection and IMG literature and has published research on IMG selection predictors for success. Her MHPE thesis studied IMG selection in Canada and her Oxford dissertation studied IMGs internationally. She recently completed a systematic review of prognostic studies on predictors for success in IMGs in postgraduate training and practice internationally as part of her Oxford dissertation. She currently sits on the Board of Directors of the Canadian Residency Matching Service as an expert in IMG matters.
Dr. Schabort was on the Ontario Steering Committee for the development of the Curriculum for the Ontario International Medical Graduate Pre-Residency program and currently is on the Curricular Advisory Committee for the Pre-residency IMG program for all RCPSC and CFPC IMGs entering residency training in Ontario. She sat on the provincial steering committee for the development of the curriculum and selection process for Practice Ready Assessment. She sat on the Steering Committee for the Ontario Inter-professional Spinal Assessment Education Clinics (ISAEC) and was the Hamilton Primary Care Lead for the implementation of the ISAEC pilot.
She has authored papers on several topics in medical education and primary care research, and an invited book chapter on International Medical Graduates. She has received several awards including the 2012 Award of Excellence from the College of Family Physicians of Canada and the Glenn Sawyer Service Award from the Ontario Medical Association in 2015 as well as the Professional Association of Residents of Ontario (PARO) Excellence in Clinical Teaching Award in 2021
Her clinical and academic interests include medical education, selection, assessment, remediation, leadership, mentorship, IMG education and advocacy, disease screening, prevention and health promotion global health, inter-professional care and education, vulnerable population health, women’s health, chronic disease management, evidence-based medicine and primary care research.
Henry Siu
MSc, MD, CCFP (COE), FCFP
Associate Professor
Medical Director, Stonechurch Family Health Centre
Henry Siu completed his undergraduate medical training at the University of Toronto in 2008, and his residency training at McMaster University in 2010. He joined the department full time in 2013 and was promoted to the rank of Associate Professor in 2020.
His clinical interests include care of the elderly, especially those living in long-term care. He currently practices at Stonechurch Family Health Centre, and as an attending physician at a local long-term care home.
His current research endeavours involve research in long-term care including auditing advance care planning rates and assessing clinicians barriers to long-term care, implementing a new periodic health examination form, and implementing a tool to support informed consent and alignment of practices in LTC to the Ontario Health Care Consent Act. He has recently received funding from the Canadian Frailty Network and Health Canada to pursue his research interests and have published articles in various journals about his work in long-term care.
Special Interests: Care of the Elderly, Long-term care
Henry Siu
MSc, MD, CCFP (COE), FCFP
Associate Professor
Medical Director, Stonechurch Family Health Centre
Henry Siu completed his undergraduate medical training at the University of Toronto in 2008, and his residency training at McMaster University in 2010. He joined the department full time in 2013 and was promoted to the rank of Associate Professor in 2020.
His clinical interests include care of the elderly, especially those living in long-term care. He currently practices at Stonechurch Family Health Centre, and as an attending physician at a local long-term care home.
His current research endeavours involve research in long-term care including auditing advance care planning rates and assessing clinicians barriers to long-term care, implementing a new periodic health examination form, and implementing a tool to support informed consent and alignment of practices in LTC to the Ontario Health Care Consent Act. He has recently received funding from the Canadian Frailty Network and Health Canada to pursue his research interests and have published articles in various journals about his work in long-term care.
Special Interests: Care of the Elderly, Long-term care
Meredith Vanstone
PhD
Associate Professor; Canada Research Chair (Tier 2) in Ethical Complexity in Primary Care
Meredith is an Associate Professor in the Department of Family Medicine and Canada Research Chair (Tier 2) in Ethical Complexity in Primary Care. She uses qualitative approaches to examine social and ethical issues related to health professional practice, education and health policy. In particular, Meredith studies how patients and primary care providers navigate socially and ethically complex care together. Socially or ethically complex care occurs in various places in primary care and Meredith has focused much of her research on complexity related to reproduction, birth, and the end of life. This work has been funded by the Canadian Institutes of Health Research, Public Health Agency of Canada, College of Family Physicians of Canada, and the Greenwall Foundation.
Meredith has a PhD in Health Professional Education from Western University, and has completed postdoctoral studies in Health Policy at McMaster University. She has provided social and ethics evidence and consulting to provincial, national, and international health policy decision-makers.
Meredith supervises graduate students with relevant research interests in the following McMaster graduate programs: Health Policy (PhD), Health Research Methodology (MSc, PhD), Health Science Education (MHSEd).
Meredith Vanstone
PhD
Associate Professor; Canada Research Chair (Tier 2) in Ethical Complexity in Primary Care
Meredith is an Associate Professor in the Department of Family Medicine and Canada Research Chair (Tier 2) in Ethical Complexity in Primary Care. She uses qualitative approaches to examine social and ethical issues related to health professional practice, education and health policy. In particular, Meredith studies how patients and primary care providers navigate socially and ethically complex care together. Socially or ethically complex care occurs in various places in primary care and Meredith has focused much of her research on complexity related to reproduction, birth, and the end of life. This work has been funded by the Canadian Institutes of Health Research, Public Health Agency of Canada, College of Family Physicians of Canada, and the Greenwall Foundation.
Meredith has a PhD in Health Professional Education from Western University, and has completed postdoctoral studies in Health Policy at McMaster University. She has provided social and ethics evidence and consulting to provincial, national, and international health policy decision-makers.
Meredith supervises graduate students with relevant research interests in the following McMaster graduate programs: Health Policy (PhD), Health Research Methodology (MSc, PhD), Health Science Education (MHSEd).
Heather Waters
BPE, MD, CCFP, FCFP
Associate Professor
Postgraduate Program Director
Dr. Heather Waters is an Associate Professor in the Department of Family Medicine at McMaster University and has been with the Department since 2000.
Dr. Waters is the Postgraduate Program Director, responsible for leading McMaster’s Family Medicine Residency Training Program across its distributed network of sites. She previously provided educational leadership in Family Medicine in the roles of Hamilton Site Director and Education Coordinator (Stonechurch Family Health Centre).
Dr. Waters works closely with program and CFPC leads in curriculum renewal through the Outcomes of Training Project (OTP). As a member of the CFPC’s Postgraduate Education Committee (PGEC), she contributes to the development of resources to support Family Medicine programs and program directors.
Dr. Waters was McMaster’s former PGME Director of Academic Performance Support and Chair of the Education Advisory Board. In these roles she provided consultation and support to residency programs, program directors, and residents in situation of learner academic difficulty and remediation. She was a founding member of the National Collaboration of Remediation Leads in 2021.
As a member of the Section of Medicine Professionalism Committee and the Professionalism in Practice Working Group at McMaster, Dr. Waters contributes to the development of tools and processes to support professionalism development for learners and faculty. As a member of the CanMeds2025 Expert Working Group on the Professional role, she is contributing to updated postgraduate competency expectations related to professionalism and professional identity formation.
Dr. Waters has a keen interest in medical education and scholarship, particularly related to postgraduate training, generalism and family medicine, professionalism and professional identity formation, humanism and the humanities in medicine, physician and resident wellness, physician leadership, and academic performance support/remediation. She is a member of McMaster’s Education Research, Innovation and Theory (MERIT) Program.
Dr. Waters has had longstanding involvement with the Foundation for Medical Practice Education and the Practice-based Small Group Learning Program (PBSG) as a board member, co-editor, author, peer and resident group facilitator.
As an expert generalist and member of the McMaster Family Health Team, Dr. Waters is actively involved in inter-professional team-based practice and education at Stonechurch Family Health Centre. She provided low risk obstetrical care through the Maternity Centre of Hamilton for twenty years, specializing in care to systemically marginalized women and their families.
Heather Waters
BPE, MD, CCFP, FCFP
Associate Professor
Postgraduate Program Director
Dr. Heather Waters is an Associate Professor in the Department of Family Medicine at McMaster University and has been with the Department since 2000.
Dr. Waters is the Postgraduate Program Director, responsible for leading McMaster’s Family Medicine Residency Training Program across its distributed network of sites. She previously provided educational leadership in Family Medicine in the roles of Hamilton Site Director and Education Coordinator (Stonechurch Family Health Centre).
Dr. Waters works closely with program and CFPC leads in curriculum renewal through the Outcomes of Training Project (OTP). As a member of the CFPC’s Postgraduate Education Committee (PGEC), she contributes to the development of resources to support Family Medicine programs and program directors.
Dr. Waters was McMaster’s former PGME Director of Academic Performance Support and Chair of the Education Advisory Board. In these roles she provided consultation and support to residency programs, program directors, and residents in situation of learner academic difficulty and remediation. She was a founding member of the National Collaboration of Remediation Leads in 2021.
As a member of the Section of Medicine Professionalism Committee and the Professionalism in Practice Working Group at McMaster, Dr. Waters contributes to the development of tools and processes to support professionalism development for learners and faculty. As a member of the CanMeds2025 Expert Working Group on the Professional role, she is contributing to updated postgraduate competency expectations related to professionalism and professional identity formation.
Dr. Waters has a keen interest in medical education and scholarship, particularly related to postgraduate training, generalism and family medicine, professionalism and professional identity formation, humanism and the humanities in medicine, physician and resident wellness, physician leadership, and academic performance support/remediation. She is a member of McMaster’s Education Research, Innovation and Theory (MERIT) Program.
Dr. Waters has had longstanding involvement with the Foundation for Medical Practice Education and the Practice-based Small Group Learning Program (PBSG) as a board member, co-editor, author, peer and resident group facilitator.
As an expert generalist and member of the McMaster Family Health Team, Dr. Waters is actively involved in inter-professional team-based practice and education at Stonechurch Family Health Centre. She provided low risk obstetrical care through the Maternity Centre of Hamilton for twenty years, specializing in care to systemically marginalized women and their families.
Department of Family Medicine Research Chairs
Canada Research Chairs
Canada Research Chairs are awarded to researchers outstanding in their field. They are awarded by the Canada Research Chair Program.
Meredith Vanstone
Tier 2 Canada Research Chair in Ethical Complexity in Primary Care
The practice of medicine relies in many ways on information gathered from clinical research and trials. But how do physicians navigate areas of care where clinical evidence doesn’t exist, is considered ambiguous, or does not play a key role in decision-making? How do they help their patients make decisions about medically complex issues?
As Canada Research Chair in Ethical Complexity in Primary Care, Meredith Vanstone aims both to improve patients’ experiences and help clinicians. She and her research team are trying to shed light on how circumstances, resources and values inform the way pregnant people navigate ethically complex decisions about reproduction. The team is approaching these goals by describing and developing educational and policy interventions to help primary care clinicians navigate complex ethical issues. Ultimately, their work will offer greater clarity to physicians and may translate into better care for patients.
Gina Agarwal
Tier 1 Canada Research Chair in Vulnerable Individuals in Primary Care
Many Canadians face challenges getting primary health care. Even when care is available, vulnerable people can have difficulties accessing it — for example, older adults or those with disabilities may find it difficult to travel to a doctor. As Canada Research Chair in Vulnerable Individuals in Primary Care, Gina Ragini Agarwal is trying to ensure that vulnerable individuals can get the health care they need, where and when they need it.
She and her research team are developing interventions to improve primary care. They are exploring new ways to measure the usefulness of health programs and developing and testing new ones. They are also running large research trials to gather evidence about the impacts of programs on individuals and health systems. Their work will lead to better access to (and more effective use of) primary care, fewer emergency visits, better health outcomes and quality of life, and a more sustainable health system.
Department Research Chairs
David Braley Nancy Gordon Chair in Family Medicine
This position was made possible by a gift from David Braley and Nancy Gordon in 2019 to support the work of outstanding faculty who are recognized internationally for their contributions to the discipline of family medicine. This individual contributes to and helps maintain our world-class reputation for excellence in family medicine — exemplifying the central values of McMaster and the Department of Family Medicine.
Their research focuses on primary care health systems, health policy, health equity and evaluating the critical relationships between primary care clinicians, teams and patients as well as other strategic research priorities of the Department.
McMaster Family Medicine Research Chair
The McMaster Family Medicine Research Chair is an internationally respected scholar working to address the challenges that face family physicians and primary care providers. Their expertise and passion for patient care is exemplified through scholarship and an established research program. The Chair engages and extends the Department’s core strengths.
In addition to contributing to the department’s research community, they also have the opportunity to teach medical students, family medicine residents and contribute to the administration of the Department.
McMaster Family Medicine Levitt Scholar
The research, interests and accomplishments of the McMaster Family Medicine Levitt Scholar focuses on primary care and further the Department’s strategic priority to advocate for and promote primary care as the foundation of strong health systems and desired health outcomes. In keeping with the legacy of Dr. Cheryl Levitt, this role is awarded to a full-time, clinical faculty member in the Department of Family Medicine who demonstrates tenacity, courage and success in creating and sustaining innovations in primary care with impact locally to globally.
Research News
Information Box Group

Spread, Implementation and Experiences of Pallium Canada’s Palliative Care ECHO Project: A Mixed Methods Evaluation
Research Project Update
February 12, 2025

Evaluation of a micro-team model at McMaster Family Practice
Research Project Update
January 27, 2025

Evaluating the CP@home program's effectiveness in reducing emergency medical services calls among frequent users
Research Project Update, VIP Lab
January 6, 2025

PoET is launching in 30 additional long term care homes
PoET Southwest Spread Project, Research Project Update
November 27, 2024

Feasibility study of an evaluation tool for tendonitis of the shoulder
Research Project Update
November 27, 2024

Assessing a medical safer supply program for people with treatment-refractory opioid use disorder
Care of PWUD, Research Project Update
November 14, 2024

Assessing barriers and facilitators to lung ultrasound use among emergency physicians
Research Project Update
November 14, 2024

New study examining palliative care awareness and training in rural family medicine postgraduate learners
Research Project Update
November 14, 2024
Research Supports and Funding
Research at the Department of Family Medicine is a broad (and growing) area of focus. To help research projects initiate, expand and share knowledge, we provide a number of resources that have been designed to help our faculty, our staff and the broader primary care research community.
Information Box Group

DFM Research Fund Learn More
The department funds projects (maximum $10,000 each) for faculty members to conduct research in primary care, palliative care and medical education.

Research Knowledge and Skill Builder Sessions Learn More
We offer monthly in-services to continue to build the research capacity of faculty and staff across the department.

TRAction: A Toolkit for Research in Action Learn More
A curated collection of resources mapped to the steps of the research process from project design to implementation and knowledge translation.

Research Group Learn More
People are at the heart of our research. We have made strategic investments to build a highly skilled staffing infrastructure to support and promote innovative primary care research involving over 15 distinct research teams.

Research Advice Café
Senior researchers offer mentorship to faculty members who are less experienced in research, providing advice and support to develop their research idea. Email pcrc@mcmaster.ca to connect.

Primary Care Research: A Pathway for Learning
This open-access online course guides learners through four steps to enhance their primary care research skills using a curated selection of tools from TRAction: A Toolkit for Research in Action. Learners can complete all four steps or select the modules that meet their specific learning needs. Please email pcrc@mcmaster.ca to access the course.
Health Sciences Library Learn More
Additional research supports are available through the Health Sciences Library for access to books, journals and e-resources and consultations with a librarian for literature search and review.
Research Leadership and Support
Our research group leadership consists of a Research Director, administrators and knowledgeable staff who support efficient, effective and high-quality research projects.
Fiona Kouyoumdjian
MD, MPH, PhD, FCFP, FRCPC
Assistant Professor
Research Director
ResearchGate
David Braley Health Sciences Centre
@F_Kouyoumdjian
fiona-kouyoumdjian-b4a2a920
McMaster Experts Profile
Fiona Kouyoumdjian is a Family Physician, Public Health and Preventive Medicine Physician, and Epidemiologist. She received her BA with Honors from Brown University, her MD from Dalhousie University, her MPH from the Johns Hopkins Bloomberg School of Public Health, and her PhD in Epidemiology from the University of Toronto Dalla Lana School of Public Health. She completed residency training at the University of Toronto and a CIHR Fellowship at St. Michael’s Hospital.
Fiona leads a program of research focused on the health status and health care of people who experience imprisonment. Her specific research foci are decreasing imprisonment, improving health care and health promotion for people in prison, and supporting successful re-integration to the community for people on release from prison.
Fiona is also an Adjunct Scientist at ICES and an Associate Member in the Department of Health Research Methods, Evidence, and Impact at McMaster.

Fiona Kouyoumdjian
MD, MPH, PhD, FCFP, FRCPC
Assistant Professor
Research Director
Laura Cleghorn
Manager, Research
Laura Cleghorn has conducted research about the organization and delivery of health care in Ontario for over 15 years in the areas of home care, primary care, and cancer care, often focused on improving access to care for marginalized populations. Since 2016, Laura has been with the Department of Family Medicine in a role that supports the faculty and staff of the Research Enterprise to engage in high-quality research. Laura is also interested in cultivating a workplace culture that encourages personal and professional growth. When not at work, Laura can be found in arenas in the greater Hamilton area, enjoying her kids’ hockey and figure skating activities. Laura’s second favourite past-time is walking her dog in Cootes Paradise, in all seasons.
Bethany Elliott
BHSc, MPH
Administrative Director, David Braley Primary Care Research Collaborative
Bethany is the Administrative Director of the David Braley Primary Care Research Collaborative (PCRC). In this role, she supports the development and expansion of a network to explore important questions in primary care and amplify evidence to inform primary care practice, education, and health systems planning. Bethany has a Master of Public Health in health promotion and community development and prior to joining the PCRC worked in the public health sector in British Columbia and Ontario for over a decade. Through this work, Bethany collaborated regularly with health system partners, local and provincial governments and community organizations on projects ranging from health promotion and evaluation to health systems planning. Most recently, she provided strategic and operational support to the Hamilton COVID-19 Response Table – a collaborative table chaired by public health, primary care, and hospitals to prevent and respond to COVID-19 in Hamilton.

Bethany Elliott
BHSc, MPH
Administrative Director, David Braley Primary Care Research Collaborative
Erin Beaulieu
RD, MPH
Manager, Knowledge Translation and Strategic Communications
Erin Beaulieu has worked for the Department of Family Medicine since March 2019 as a Knowledge Translation (KT) Specialist and then moved into the role of KT and Strategic Communications Manager in February 2022. In this role, she provides leadership, guidance and support for targeted, responsive and effective KT and communications initiatives across all departmental domains to further strategic objectives, strengthen internal and external engagement, enable greater research impact by furthering the uptake of evidence into practice and policy. Prior to joining McMaster University, Erin worked as a Registered Dietitian in public health and supporting local food policy and programs in the provincial government. Erin holds a Bachelor of Applied Science in Applied Human Nutrition and a Masters of Public Health in Community Nutrition. When she’s not at work, Erin enjoys cooking, cycling, and cuddling with her cat, Ollie.

Erin Beaulieu
RD, MPH (on leave)
Manager, Knowledge Translation and Strategic Communications
Information Box Group
Neha Arora
Clinic Research Coordinator
Neha has been a part of McMaster since 2011 working in DFM since 2014 on the iGAP study. She is a trained physiotherapist and her research interests are in the care of the elderly.
Brittney Bowen
Administrative Assistant
Patricia Habran-Dietrich
BA
Administrative Assistant (on LOA)
Patricia Habran-Dietrich joined McMaster in 2013, as an administrative assistant for the Aging, Community and Health Research Unit (ACHRU), within the School of Nursing. In mid- 2014, Patricia joined the Department of Family Medicine as part of the HOPE program. Since 2015 she has been a member of the Research Enterprise, providing direct support to Drs. Dee Mangin and Michelle Howard in their research administrative tasks, as well as broadly supporting the staff of the research team.
Her broad interests include travel, reading and meeting people from diverse backgrounds.

Patricia Habran-Dietrich
BA
Administrative Assistant (on LOA)
Casey Irvin
MA
Manager, Knowledge Translation and Strategic Communications
Casey Irvin works to amplify our department’s impact.
As the manager of knowledge translation and strategic communications at the department of family medicine (DFM), he supports faculty, staff and learners to help connect their ideas, research and purpose to key audiences.
Casey worked with DFM for six years as both a communications coordinator and as the department’s first knowledge translation specialist before joining the McMaster Institute for Research on Aging in 2021. Returning to DFM in 2024 (to cover a leave for Erin Beaulieu), Casey is a steadfast advocate for creating progressive, equitable improvements to health care through effective communication, knowledge mobilization and telling good stories.
He has a master’s degree in communications and cultural studies and over 15 years of communications experience in the health care, education and social services sectors.
Advina Kamaric
MPH
Knowledge Translation Specialist
Advina Kamaric has been working for the Department of Family Medicine since July 2023. In her role as Knowledge Translation Specialist, she works with DFM researchers to raise awareness of the outcomes of research projects in the department through the development of various knowledge translation products such as infographics, videos, reports, and social media posts.
Advina holds a Bachelor of Science in Health Studies with a Specialization in Health Research and a Master of Public Health.
Outside of work, Advina enjoys traveling, baking, and reading.
Jennifer Salerno
MSc, PhD
Research Associate
Dr. Jennifer Salerno’s research interests include chronic disease epidemiology and the application of epidemiology methods to trial research, population and public health, and health services research. She holds a PhD in Epidemiology from the University of Toronto, MSc in Community Health and Epidemiology from Queen’s University, and Honours BSc from McMaster University’s Biology and Pharmacology Co-operative Program. She completed fellowship training at both the Toronto Rehabilitation Institute in the area of traumatic brain injury epidemiology and the U.S. National Institutes of Health (National Cancer Institute’s Hormonal and Reproductive Epidemiology Branch) in the area of breast cancer epidemiology. Her previous research interests included studying the epidemiology of brain injuries and related vascular dementias, and specifically, examining the etiology of cognitive function in aging populations using molecular/biochemical methods and advanced statistical models. She previously worked for several years as a clinical epidemiologist in the Government of Ontario (MOHLTC and Health Quality Ontario) where she performed several health technology assessments, systematic reviews and meta-analyses. She also developed cancer clinical practice guidelines supporting Cancer Care Ontario’s Cancer Imaging Program through McMaster’s Program in Evidence-Based Care, Department of Oncology.
Currently, at McMaster University, she is a Research Associate for the Department of Family Medicine. She is involved in the TAPER research study (TAPER: Team Approach to Polypharmacy Evaluation and Reduction) which aims to reduce multiple medication use and the harmful effects of polypharmacy among older adults. She is also involved with the Primary Care Research Collaborative (PCRC) in the Department of Family Medicine by providing clinical faculty teaching and mentoring initiatives and opportunities and developing the patient/public/community advisory group for the PCRC. She currently teaches in the health research methodology program in the Department of Health Research Methods, Evidence, and Impact at McMaster and is currently the Vice Chair of the American College of Epidemiology (ACE) Ethics Committee. She has held numerous leadership positions in ACE and more recently, she is involved with the International Epidemiological Association as the North American Regional Councillor.
Michelle Sylvain
Administrative Coordinator
Michelle joined McMaster’s Department of Family Medicine in August 2019 as the Research Administrative Coordinator. She transitioned to administrative work in 2015 after 10 years in broadcasting. Michelle enjoys cooking in her spare time and travelling whenever possible.
Neha Arora
Clinic Research Coordinator
Neha has been a part of McMaster since 2011 working in DFM since 2014 on the iGAP study. She is a trained physiotherapist and her research interests are in the care of the elderly.
Neha Arora
Clinic Research Coordinator
Neha has been a part of McMaster since 2011 working in DFM since 2014 on the iGAP study. She is a trained physiotherapist and her research interests are in the care of the elderly.
Brittney Bowen
Administrative Assistant
Brittney Bowen
Administrative Assistant
Patricia Habran-Dietrich
BA
Administrative Assistant (on LOA)
Patricia Habran-Dietrich joined McMaster in 2013, as an administrative assistant for the Aging, Community and Health Research Unit (ACHRU), within the School of Nursing. In mid- 2014, Patricia joined the Department of Family Medicine as part of the HOPE program. Since 2015 she has been a member of the Research Enterprise, providing direct support to Drs. Dee Mangin and Michelle Howard in their research administrative tasks, as well as broadly supporting the staff of the research team.
Her broad interests include travel, reading and meeting people from diverse backgrounds.
Patricia Habran-Dietrich
BA
Administrative Assistant (on LOA)
Patricia Habran-Dietrich joined McMaster in 2013, as an administrative assistant for the Aging, Community and Health Research Unit (ACHRU), within the School of Nursing. In mid- 2014, Patricia joined the Department of Family Medicine as part of the HOPE program. Since 2015 she has been a member of the Research Enterprise, providing direct support to Drs. Dee Mangin and Michelle Howard in their research administrative tasks, as well as broadly supporting the staff of the research team.
Her broad interests include travel, reading and meeting people from diverse backgrounds.
Casey Irvin
MA
Manager, Knowledge Translation and Strategic Communications
Casey Irvin works to amplify our department’s impact.
As the manager of knowledge translation and strategic communications at the department of family medicine (DFM), he supports faculty, staff and learners to help connect their ideas, research and purpose to key audiences.
Casey worked with DFM for six years as both a communications coordinator and as the department’s first knowledge translation specialist before joining the McMaster Institute for Research on Aging in 2021. Returning to DFM in 2024 (to cover a leave for Erin Beaulieu), Casey is a steadfast advocate for creating progressive, equitable improvements to health care through effective communication, knowledge mobilization and telling good stories.
He has a master’s degree in communications and cultural studies and over 15 years of communications experience in the health care, education and social services sectors.
Casey Irvin
MA
Manager, Knowledge Translation and Strategic Communications
Casey Irvin works to amplify our department’s impact.
As the manager of knowledge translation and strategic communications at the department of family medicine (DFM), he supports faculty, staff and learners to help connect their ideas, research and purpose to key audiences.
Casey worked with DFM for six years as both a communications coordinator and as the department’s first knowledge translation specialist before joining the McMaster Institute for Research on Aging in 2021. Returning to DFM in 2024 (to cover a leave for Erin Beaulieu), Casey is a steadfast advocate for creating progressive, equitable improvements to health care through effective communication, knowledge mobilization and telling good stories.
He has a master’s degree in communications and cultural studies and over 15 years of communications experience in the health care, education and social services sectors.
Advina Kamaric
MPH
Knowledge Translation Specialist
Advina Kamaric has been working for the Department of Family Medicine since July 2023. In her role as Knowledge Translation Specialist, she works with DFM researchers to raise awareness of the outcomes of research projects in the department through the development of various knowledge translation products such as infographics, videos, reports, and social media posts.
Advina holds a Bachelor of Science in Health Studies with a Specialization in Health Research and a Master of Public Health.
Outside of work, Advina enjoys traveling, baking, and reading.
Advina Kamaric
MPH
Knowledge Translation Specialist
Advina Kamaric has been working for the Department of Family Medicine since July 2023. In her role as Knowledge Translation Specialist, she works with DFM researchers to raise awareness of the outcomes of research projects in the department through the development of various knowledge translation products such as infographics, videos, reports, and social media posts.
Advina holds a Bachelor of Science in Health Studies with a Specialization in Health Research and a Master of Public Health.
Outside of work, Advina enjoys traveling, baking, and reading.
Jennifer Salerno
MSc, PhD
Research Associate
Dr. Jennifer Salerno’s research interests include chronic disease epidemiology and the application of epidemiology methods to trial research, population and public health, and health services research. She holds a PhD in Epidemiology from the University of Toronto, MSc in Community Health and Epidemiology from Queen’s University, and Honours BSc from McMaster University’s Biology and Pharmacology Co-operative Program. She completed fellowship training at both the Toronto Rehabilitation Institute in the area of traumatic brain injury epidemiology and the U.S. National Institutes of Health (National Cancer Institute’s Hormonal and Reproductive Epidemiology Branch) in the area of breast cancer epidemiology. Her previous research interests included studying the epidemiology of brain injuries and related vascular dementias, and specifically, examining the etiology of cognitive function in aging populations using molecular/biochemical methods and advanced statistical models. She previously worked for several years as a clinical epidemiologist in the Government of Ontario (MOHLTC and Health Quality Ontario) where she performed several health technology assessments, systematic reviews and meta-analyses. She also developed cancer clinical practice guidelines supporting Cancer Care Ontario’s Cancer Imaging Program through McMaster’s Program in Evidence-Based Care, Department of Oncology.
Currently, at McMaster University, she is a Research Associate for the Department of Family Medicine. She is involved in the TAPER research study (TAPER: Team Approach to Polypharmacy Evaluation and Reduction) which aims to reduce multiple medication use and the harmful effects of polypharmacy among older adults. She is also involved with the Primary Care Research Collaborative (PCRC) in the Department of Family Medicine by providing clinical faculty teaching and mentoring initiatives and opportunities and developing the patient/public/community advisory group for the PCRC. She currently teaches in the health research methodology program in the Department of Health Research Methods, Evidence, and Impact at McMaster and is currently the Vice Chair of the American College of Epidemiology (ACE) Ethics Committee. She has held numerous leadership positions in ACE and more recently, she is involved with the International Epidemiological Association as the North American Regional Councillor.
Jennifer Salerno
MSc, PhD
Research Associate
Dr. Jennifer Salerno’s research interests include chronic disease epidemiology and the application of epidemiology methods to trial research, population and public health, and health services research. She holds a PhD in Epidemiology from the University of Toronto, MSc in Community Health and Epidemiology from Queen’s University, and Honours BSc from McMaster University’s Biology and Pharmacology Co-operative Program. She completed fellowship training at both the Toronto Rehabilitation Institute in the area of traumatic brain injury epidemiology and the U.S. National Institutes of Health (National Cancer Institute’s Hormonal and Reproductive Epidemiology Branch) in the area of breast cancer epidemiology. Her previous research interests included studying the epidemiology of brain injuries and related vascular dementias, and specifically, examining the etiology of cognitive function in aging populations using molecular/biochemical methods and advanced statistical models. She previously worked for several years as a clinical epidemiologist in the Government of Ontario (MOHLTC and Health Quality Ontario) where she performed several health technology assessments, systematic reviews and meta-analyses. She also developed cancer clinical practice guidelines supporting Cancer Care Ontario’s Cancer Imaging Program through McMaster’s Program in Evidence-Based Care, Department of Oncology.
Currently, at McMaster University, she is a Research Associate for the Department of Family Medicine. She is involved in the TAPER research study (TAPER: Team Approach to Polypharmacy Evaluation and Reduction) which aims to reduce multiple medication use and the harmful effects of polypharmacy among older adults. She is also involved with the Primary Care Research Collaborative (PCRC) in the Department of Family Medicine by providing clinical faculty teaching and mentoring initiatives and opportunities and developing the patient/public/community advisory group for the PCRC. She currently teaches in the health research methodology program in the Department of Health Research Methods, Evidence, and Impact at McMaster and is currently the Vice Chair of the American College of Epidemiology (ACE) Ethics Committee. She has held numerous leadership positions in ACE and more recently, she is involved with the International Epidemiological Association as the North American Regional Councillor.
Michelle Sylvain
Administrative Coordinator
Michelle joined McMaster’s Department of Family Medicine in August 2019 as the Research Administrative Coordinator. She transitioned to administrative work in 2015 after 10 years in broadcasting. Michelle enjoys cooking in her spare time and travelling whenever possible.
Michelle Sylvain
Administrative Coordinator
Michelle joined McMaster’s Department of Family Medicine in August 2019 as the Research Administrative Coordinator. She transitioned to administrative work in 2015 after 10 years in broadcasting. Michelle enjoys cooking in her spare time and travelling whenever possible.




















