Overview
Our program is spread across Southern Ontario in both urban and community hospitals. Learners have direct clinical exposure and provide emergency medicine care for adults, children, elderly and special populations that commonly use Canadian emergency medical services. The teaching hospitals used are organized by specialty, such as burn/trauma, oncology, pediatric trauma, and emergency psychiatry. The hospitals offer emergency departments supported by comprehensive medical and surgical services.
Education is both didactic and hands on and our approach to teaching encourages the development of competency in emergency medicine care for a wide range of pathology. We use ongoing competency assessment and foster an environment of continued assessment and improvement. We have a competency committee that collaborates with the learner to encourage specific structured learning off-shift to augment the clinical learning experience.
Expandable List
Simulation – The simulation curriculum offers at least 10 – 12 sessions per academic year. Residents will tackle complex medical cases and hone skills in communication, leadership, and resource utilization. We are also working to implement a more robust pediatric simulation curriculum to ensure more exposure to challenging low frequency, high equity cases. Sessions are led by staff with simulation expertise and use high fidelity mannequins.
Tintinalli Rounds – These sessions are designed to be more interactive and focus on clinical process opposed to spending significant time on pathophysiology.
Clinical Skills – Clinical skills sessions occur throughout the year. Sessions include a day in the anatomy lab practicing on cadavers, at least 4 simulation sessions with high fidelity mannequins, orthopedic casting sessions and CT head sessions.
Practice Orals – There will be regularly scheduled practice oral sessions throughout the academic year. During these sessions faculty will deliver a practice oral to you that will closely mimic the environment of the orals during your EM examination.
Written Examinations – You will be given a sample exam at least twice per academic year as well as a National In-Training Practice Exam that will be written in the Spring of your academic year.
Journal Club – The program runs monthly Journal Club sessions to assist in the development of the resident’s critical appraisal skills.
Ultrasound – You will be provided with an Ultrasound Boot-Camp in the fall of your academic year. This course includes a pre-course online, practical course and written exam. You will also have an advanced Ultrasound Day following your certification. This session will expose you to resuscitation and advanced ultrasound scans in a case-based format, covering a condensed version of many advanced scans. There are remote virtual POCUS rounds with an optional and mandatory component.
Longitudinal Rounds (ECG) – weekly virtual rounds on ECG and cardiology-focused topics
Scholarly Work and Research Project – A program requirement is supported by the Department of Family Medicine and Division of Emergency Medicine to develop scholarly work such as research, teaching, interprofessional collaboration and teaching throughout the third-year program.
The application process will run through the CARMS match. The website will be available at carms.ca. All applicants for the Family Medicine/Emergency Medicine Residency Program are required to:
- Complete the National Application form
- Complete the National Match Registration Form
- Provide three letters of reference and Referee Assessment forms
- Provide a Family Medicine Program Director’s Assessment of Applicant form
- Written letter to Dr. Alexandra Mitcham, Program Director, Family Medicine/Emergency Medicine Residency program stating your reasons for wishing to join this program
- Send a curriculum vitae
The Selection Committee will be chaired by the Program Director and will consist of resident representatives and faculty members from the Residency Steering Committee. For application deadlines and interview dates, please refer to the CaRMS website.
Emergency Medicine Education
This one-year residency program designates learners as a third-year resident in the Family Medicine/Emergency Medicine Program. Rotations include ICU, CCU, Trauma, Plastic and Emergency Medicine. Over the total three years of training, residents must complete a minimum of eight blocks of training in the emergency department with a minimum of four blocks in the third year. One of the eight blocks will include significant experience in emergency pediatrics, obtained at McMaster Children’s Hospital. Candidates are urged to make use of their elective time in the first or second year of their family medicine residency to enroll in some of the above rotations.
Expandable List
Residents can direct some of the schedule of their one-year emergency medicine training. However, certain rotations are considered mandatory and must be completed under any of the training formula.
A “typical” residency year would include:
- 4 blocks – Emergency Medicine
- 1 block – Emergency Pediatrics
- 1 block – Community Emergency Medicine
- 1 block – Trauma / Acute Care Surgery
- 2 blocks – ICU
- 1 block – CCU
- 1 block – Selective
- 1 block – Anesthesia
- 1 block – Plastics/orthopedics
Selectives
Selectives are tailored towards the resident’s stated objectives and can be completed in a variety of formats, and approval is based on a set of criteria. In the past, selectives have included Toxicology in New York City (varying availability), or an additional block of Trauma, Emergency or Surgery.
Rotations may be tailored to your prior training and career goals, however, certain rotations are considered mandatory and must be completed. Rotations will include ICU, CCU, Surgery, Trauma, Orthopedics, Plastics and Emergency Medicine.
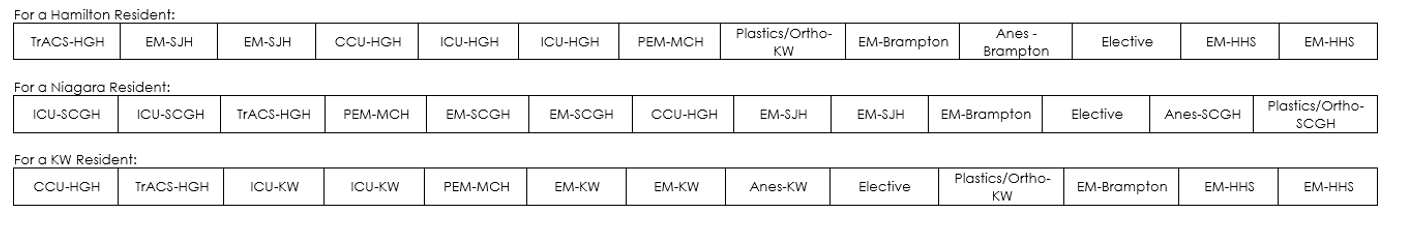
Please note: These are sample schedules. Communities and Academic Centers as well as rotation type can be modified.
Emergency medicine core content material is presented at the weekly academic day, which takes place on Thursdays. Core content topics include radiology, examination preparation, bioethics, and administration.
In addition, there will be multiple Simulation Sessions with high fidelity simulators through the academic year. Finally, there is a day in the Anatomy Lab practicing procedures on cadavers.
Academic day program includes:
- Tintinalli Rounds
- Procedural Skills Session
- Practice Oral Examination
- Practice Written Examination
- ECG rounds
Residents are required to attend a monthly Journal Club. EMS rideouts will be performed during the Emergency Medicine block, 2 days.
Residents are expected to complete a research project on evidence-based medicine skills, for which they will search databases, critically appraise the articles and present the material at a resident research day. This may take the form of a CQI/QA project; literature search or a formal research design study. It is expected that residents will display competence in preparing, practicing and evaluating evidence-based medicine. Other aspects of scholarly work including teaching, interprofessional collaboration and leadership are also included / considered.
An ultrasound course following the national principles is offered in the early fall of the EM year. This course teaches the technical skills and didactic principles of Point of Care Ultrasound (POCUS). The remainder of the course is spent scanning volunteers to achieve the required number of scans. We have ample faculty available to assist with attaining the required scans for full certification if unable during the course in ultrasound. A second advanced ultrasound course will be completed in the spring of the EM year. There are longitudinal options for POCUS on emergency medicine blocks.
At the start of the academic year each resident is connected to a Faculty Mentor to support learning and career goals. There are many opportunities to engage with our Royal College colleagues, including several social events. In addition, the annual Resident Retreat is organized with EM Faculty.
Applicants must have successfully completed two years of a Family Medicine Residency Program leading to certification by the College of Family Physicians of Canada. Applicants must also have written, or be eligible to write, the College of Family Physicians of Canada Certification Examination.
Emergency Medicine Contacts
Dr. Alexandra Mitcham
Program Director, Division of Emergency Medicine
Department of Family Medicine
alexandra.mitcham@medportal.ca
Dr. Liane Shipp-Dey
Director, Division of Emergency Medicine
Department of Family Medicine
liane.shipp-dey@medportal.ca
Dr. Kyle Dorosh
Assistant Program Director, Division of Emergency Medicine
Department of Family Medicine
kyle.dorosh@medportal.ca
Kelly Binkle
Program Administrator, Enhanced Skills Emergency Medicine Program
Department of Family Medicine
kbinkle@mcmaster.ca
Bronwyn Andrews
PGY-1 Core and Emergency Medicine Electives
Hamilton Emergency Departments (SJH, HGH, JHCC)
emctu@mcmaster.ca
Dr. Kayleigh Hagerman
Regional Education Coordinator
Niagara Regional Campus
CCFP Emergency Medicine Residency Program
kayleigh.hagerman@medportal.ca
Dr. Adrianna Arkilander
Regional Education Coordinator
Kitchener Waterloo Regional Campus
CCFP Emergency Medicine Residency Program
adrianna.arkilander@medportal.ca

